Background Knowledge:
-------------------------------------------------------
Semicircular canal has three components:
anterior(superior), posterior, lateral(horizontal) canal
Posterior canal BPPV — The Dix-Hallpike maneuver
--------------------------------------------------------------
Method:
- The patient's head is turned 45° towards the ear being tested.
- The head is supported, and then the patient is quickly lowered into the supine position with the head extending about 30° below the horizontal while remaining turned 45° towards the ear being tested.
- The head is held in this position and the physician checks for nystagmus.
- To complete the manoeuvre, the patient is returned to a seated position and the eyes are again observed for reversal nystagmus.
Interpretation (Positive Hallpike test):
Head is turned to the right, to test the right ear.
If the right ear is affected, nystagmus occurs as described below:
A: When the head is lowered 30 degree below the bed,
the fast phase of the nystagmus is upward , rotating toward the affected ear
B: When the patient is brought back to the sitting position,
the fast phase of the nystagmus is downward , rotating toward the affected ear
Anterior canal BPPV - The Dix-Hallpike maneuver
--------------------------------------------------------------
Method:
- same as posterior canal BPPV
Interpretation:
In positive Hallpike test, the nystagmus is downbeat and torsional(rotational), with the top of the eye torting away from the lower ear.
Treatment of Posterior or Anterior canal BPPV
--------------------------------------------------------------
Two methods: Epley maneuver and Semont maneuver
Epley maneuver
/////////////////
Place the patient in a sitting position on the end of the examination table.
Rotate the head 45° towards the affected ear, then swiftly place the patient in a supine position with the head hanging 30° below the horizontal at the end of the examining table (Dix-Hallpike position).
Observe for nystagmus and hold the position for ~30 seconds after it stops.
The head is rotated 90° towards the opposite ear while maintaining the head hanging position.
Observe for nystagmus and hold the position for ~30 seconds after it stops.
Continue then to roll the whole patient another 90° towards the unaffected side until their head is facing 180° from the original Dix-Hallpike position. This change in position should take <3 to 5 seconds.
Observe for nystagmus and hold the position for ~30 seconds after it stops.
Then have the patient sit up. Upon sitting, there should be no vertigo or nystagmus in a successful manoeuvre, because the particles will have been cleared from the posterior semicircular canal back into the utricle.
If there is not paroxysmal nystagmus or symptoms during Dix-Hallpike positioning (Steps 1, 2) then there is a high likelihood of success.
/////////////////
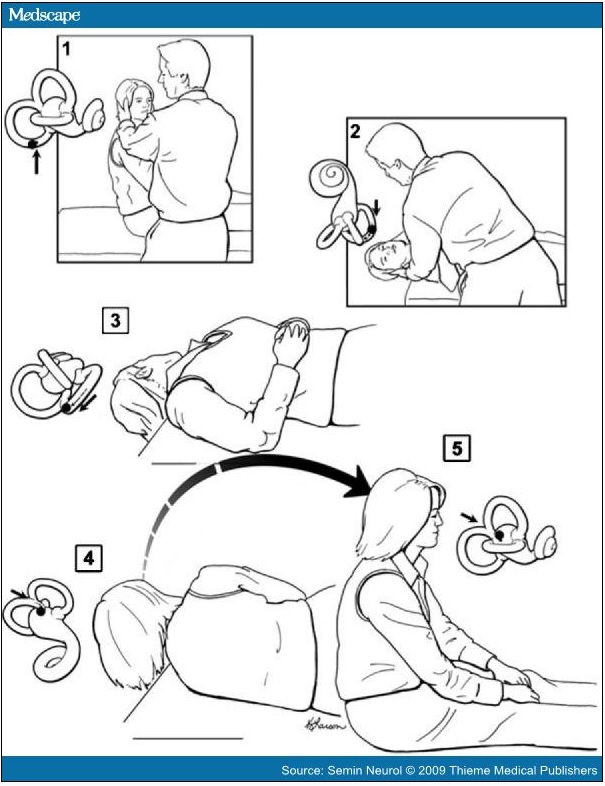
Semont maneuver
////////////////
Sit the patient midway along the long side of an examination table, with their legs hanging over the edge.
Rotate the head 45° towards the unaffected side. While maintaining the head rotation, swiftly place the patient's upper body in a side-lying position on the affected side, with the head resting on the examination table and now facing upwards. This may induce nystagmus and vertigo because of particle movement towards the apex of the semicircular canal. Maintain this position until the vertigo and nystagmus stop (1 to 2 minutes).
Move the patient rapidly through the sitting position of step 1 and into the opposite side-lying position while maintaining the same head rotation, so that the head is resting on the examination table and now facing downwards. A nystagmus response in the same direction would indicate that the particles are exiting the semicircular canal. The transition from step 2 to 3 relies on inertia, and therefore it must be done very quickly. Maintain this position until the vertigo and nystagmus stop (1 to 2 minutes). Slowly return the patient to the sitting position of step 1.
Lateral(Horizontal) canal BPPV - Supine head turn maneuver
--------------------------------------------------------------
The nystagmus of horizontal canal BPPV, unlike that of posterior canal BPPV, is distinctly horizontal(moving to the left and or to the right, i.e. not up and down) and changes direction with changes in head position. There is no torsional(rotational) component.
The paroxysmal direction changing nystagmus may be either geotropic or apogeotropic.
Geotropic direction-changing positional nystagmus is right beating upon turning the head to the right and then left beating when turning the head back to the left side. (geotropic nystagmus = nystagmus "towards ground")
Conversely, the apogeotropic form indicates the nystagmus is right beating with turning to the left and left beating with turning to the right. (apogeotropic nystagmus = nystagmus "away from ground")
In geotropic nystagmus,
The downward ear, on the side where the nystagmus is more intense = the affected ear.
In apogeotrpic nystagmus,
The downward ear, on the side where the nystagmus is less intense = the affected ear.
{그냥 쉽게 병변 쪽으로 nystagmus 가 더 심하게 흘겨 본다고 보면 됨}
The latency is often brief, and the duration may be 15 to 60 seconds. This nystagmus appears less apt to fatigue with repeat
positioning than in cases of posterior canal BPPV; consequently, patients are more likely to become ill with attempts to fatigue this
form of BPPV.
(There is speculation that apogeotropic direction-changing nystagmus suggests cupulolithiasis, and geotropic nystagmus
suggests canalithiasis as the mechanism.)
Treatment of Lateral(Horizontal) canal BPPV
--------------------------------------------------------------
Lempert roll maneuver
////////////////////////
Lempert 360- (Barbeque) degree roll maneuver to treat horizontal canal BPPV. When the patient's head is positioned with the affected ear down, the head is then turned quickly 90 degrees toward the unaffected side (face up). A series of 90-degree turns toward the unaffected side is then undertaken sequentially until the patient has turned 360 degrees and is back to the affected ear-down position. From there, the patient is turned to the face-up position and then brought up to the sitting position. The successive head turns can be done in 15- to 20-second intervals even when the nystagmus continues. Waiting longer does no harm, but may lead to the patient developing nausea, and the shorter interval does not appear to detract from the effectiveness of the treatment.
////////////////////////
Gufoni maneuver
////////////////////////
(1) patient seated on the examination couch with both the legs hanging out from the same side, arms held close to the body, and
hands resting on the knees
(2) patient is then made to lie down on the uninvolved lateral side with a quick lateral movement and maintained in this position for 2
minutes until the end of evoked geotropic nystagmus
(3) quick 45° rotation of the head towards the floor, position being maintained for 2 minutes
(4) slow return back to the starting position
////////////////////////
Chracteristics of BPPV:
---------------------------------
- The latency, transience, and fatigability of the nystagmus
(latency - few seconds (2~5 sec)
transience - usu. lasts less than 30 sec
fatigability - nystagmus / diziness weakens with repeted maneuver)
- Typical mixed upbeat/downbeat + torsional(rotational) nystagmus
Characteristics of Central disorder:
---------------------------------
Latency - none
duration of nystagmus - greater than 1 minute
not-fatiguing
(videos:
Post/Ant canal BPPV
http://www.youtube.com/watch?v=59EIKztATiw
http://www.youtube.com/watch?v=LsPURdtMjac
Laterl canal BPPV
http://www.youtube.com/watch?v=iOJOArGmepM
http://balancemd.net/Horizontal_Canal_BPPV.html)