Stroke
Classified into two types:
1) Ischaemic
2) haemorrhagic
Ischamic stroke:
=====================
is either - thrombotic or embolic
thrombotic - from ahterosclerosis
embolic - from heart or from aneurysm
Symp:
----------------
monocular vision loss, visual field loss
unilateral (facial/limb) weakness
aphasia (impaired language function - sign of dominant hemispheric ischaemia)
ataxia
{symp mem tip below}
Test:
----------------
CT brain (mainly to exclude hemorrhagic stroke. CT brain may be normal within first few hours of ischaemic stroke.
Rx:
----------------
presentation within 3 hrs and no contraindication to thrombolytics -> tPA (ateplase)
presentation after 3 hrs -> aspirin 300 mg dly
cerebral venous sinus thrombosis -> heparin / warfarin
DVT prophylaxis
haemorrhagic stroke
=====================
Symp:
----------------
Headache ("most severe headache of my life" suggests subarachnoid haemorrahge)
Neck stiffness
Visual impairment (hemianopia(half visual field defect), diplopia), photophobia
Unilateral (face/limb) weakness
Seonsory loss
Aphasia (impaired language function - sign of dominant hemispheric ischaemia)
Dysarthria, ataxia
Nausea/vomiting (uncommon)
Altered level of consciousness/confusion (uncommon)
{symp mem tip below}
Test:
----------------
CT brain
INR
Rx:
----------------
-Airway protection (Intubate if GCS <= 8)
-Sedation (with propofol/midazolam/barbiturate - e.g. in ICU setting - midazolam 0.1 mg/kg (typically 5 mg) ivi as a loading dose,
then 0.1 mg/kg/hr)
-Anticonvulsant (phenytoin 15 mg/kg over 20 min loading, then 3 mg/kg 12hrly)
-Antipyretic (paracetamol)
-BP control ( pt often have sys BP > 180. keep sys BP just below 160 using labetalol. CAUTION - too low BP may worsen the
damage)
-Treat hyperglycemia (if serum glucose > 10 mmol/L)
-Head 30 degree elevated at bed.
-Mannitol 1g/kg IV bolus, maintenance 0.25 ~ 0.5 g /kg every 6 hrs.
-Correct coagulopathy if it exists.
Neurosurg consult
{mem tip:
Airway, Sedation, -ABC
Head 30 degree, mannitol, -압력 낮춰 공급높이고
Hypertension, Diabetes, Epilepsy -대사활동 줄여 소모줄이고
}
{symp mem tip:
//////////////
Cincinnati prehospital stroke scale:
==================================
- Facial drop (seen by asking the pt to - "show me your teeth")
- Arm drift ( hold out two arms with palms up and eyes closed for 10 sec. one arm drifts down)
- Abnormal speech ( have the pt say "you can't teach an old dog new tricks" - pt slurs words/uses wrong words/can't speak)
if one of the above positive - 75 % chance of stroke
if all three positive - more than 85 % chance of stroke
/////////////
stroke (both hemorrhagic & ischaemic) - cincinnati scale 에 시력/시야 검사 더함.
Visual impairment:
-ischaemic stroke: monocular blindness, visual field defect
-hemorrhagic stroke: hemianopia(half visual field defect), diplopia
Hemorrhagic stroke 에는 다음과 같은 특징이 더함.
Characteristic of hemorrhagic stroke:
-Headahce (common but may be absent)
-Neck stiffness (common)
-nausea/vomiting (uncommon)
-altered level of consciousness (uncommon)
즉,
마치 memnigitis 같이 - neck stiffness, headache, nausea vomitting
바보같은 radiologist 는 GCS 15/15 은 hemorrhage 아니라고 하겠지만 hemorrhagic stroke 가 꼭 혼수상태일 필욘 없음.
다만 GCS 가 낮으면 mortality 가 높아짐. Haemorrhage size 가 커도 mortality 높아짐
이 블로그 검색
2013년 6월 26일 수요일
Neuroleptic malignant syndrome
Neuroleptic malignant syndrome
===============================
Hx:
-----------
Exposure to antipsychotic medications,
Abrupt withdrawal of dopaminergic drugs, and
Structural brain abnormality.
Symp:
-----------
Altered mental status (confusion, psychosis, delirium)
Muscle rigidity (lead pipe or generalized hypertonia)
Hypertension, hypotension, tachycardia
Diaphoresis, sialorrhoea, urinary incontinence
Fever
{mem tip
머리가 굳고 (altered mental status)
몸이 굳는다 (rigidity)
몸이 굳어 혈압 상승. 몸이 굳어 열이남.
여러군데서 물이 샘 (diaphresis - 땀, sialorrhea - 침, urinary continence - 오줌)
}
Test:
-----------
elevated CK (>500 units/L)
Other metabolic panel often normal.
Rx:
-----------
Stop antipsychotic, dopaminergic antagonist. Restart/continue dopamine agonist.
rhabdomyolysis - vigorous hydration with IV fluid
Hyperthemia - paracetamol / ibprofen
dantrolene(controversial, may prolong clinical recovery) 1mg/kg IVI once. (over 1 hr)
===============================
Hx:
-----------
Exposure to antipsychotic medications,
Abrupt withdrawal of dopaminergic drugs, and
Structural brain abnormality.
Symp:
-----------
Altered mental status (confusion, psychosis, delirium)
Muscle rigidity (lead pipe or generalized hypertonia)
Hypertension, hypotension, tachycardia
Diaphoresis, sialorrhoea, urinary incontinence
Fever
{mem tip
머리가 굳고 (altered mental status)
몸이 굳는다 (rigidity)
몸이 굳어 혈압 상승. 몸이 굳어 열이남.
여러군데서 물이 샘 (diaphresis - 땀, sialorrhea - 침, urinary continence - 오줌)
}
Test:
-----------
elevated CK (>500 units/L)
Other metabolic panel often normal.
Rx:
-----------
Stop antipsychotic, dopaminergic antagonist. Restart/continue dopamine agonist.
rhabdomyolysis - vigorous hydration with IV fluid
Hyperthemia - paracetamol / ibprofen
dantrolene(controversial, may prolong clinical recovery) 1mg/kg IVI once. (over 1 hr)
2013년 6월 24일 월요일
Testicular torsion / Epididymitis
Three main differential Dx of painful testis: Testicular torsion, epididymitis, orchitis
Testicular torsion:
==================
Symp:
-----------------------
High riding testicle
{mem tip: 말려 올라갔으니까}
No pain relief upon elevation of scrotum
{mem tip: 벌써 올라가있으니까 - 내가 올려본다}
(if pt experience pain relief with elevation of the testis (Prehn sign) -> suggests epididymitis more than torsion)
Absent cremasteric reflex(elevation of the testis in response to stroking of the upper inner thigh)
(it also may be absent in boys without torsion, particularly if they are younger than six months)
{mem tip: 벌써 올라가있으니까 - 환자의 근육이 올린다}
The testis may be lying horizontally, displacing the epididymis from its normal posterolateral position.
Scrotal swelling/edema
Nausea vomiting
(Nearly 90 percent of patients may have associated nausea and vomiting)
Dx:
-----------------------
Scrotal ultrasound (Collour doppler)
Abnormal urinalysis suggests epididymitis/orchitis more than testicular torsion
Rx:
-----------------------
- Analgesia
- immediate urological consultation for emergency scrotal exploration
Typical rates of viability:
* Detorsion within 4 to 6 hours — 100 percent viability
* Detorsion after 12 hours — 20 percent viability
* Detorsion after 24 hours — 0 percent viability
- if surgery is not available within 6 hours [13] or while preparations for surgery are being made -> manual de-torsion
Manual de-torsion is a temporising measure. The technique involves rotating the right testicle counter-clockwise and the left testicle
clockwise. In other words, the affected testicle is rotated as if opening a book, hence the 'open book' method.
Epididymitis
===================
Symps
--------------
Pain and swelling typically develops over the course of a few days (unlike testicular torsion, which is usually of sudden onset).
The affected testis has a normal vertical lie
Pt may experience pain relief with elevation of the testis (Prehn sign)
Painful micturition (uncommon)
urethral discharge (uncommon)
Epididymitis is caused by organisms causing UTI/STI.
Rx:
--------------
Sexually transmitted:
-cetriaxone 250 mg IMI stat AND
-doxycycline 100 mg BD PO for 14 days
(NOTE: Doxycycline is not approved for use in children younger than the age of eight years)
Not sexually transmitted:
-empiric quinolone: ofloxacin 300 mg BD PO for 10 days OR levofloxacin 500 mg dly PO for 10 days
(NOTE: Fluoroquinolones are not approved for use in patients younger than 18 years of age when other effective alternatives are available)
Prog
--------------
Swelling of testis from epididymitis may takes a month or more to subside
Testicular torsion:
==================
Symp:
-----------------------
High riding testicle
{mem tip: 말려 올라갔으니까}
No pain relief upon elevation of scrotum
{mem tip: 벌써 올라가있으니까 - 내가 올려본다}
(if pt experience pain relief with elevation of the testis (Prehn sign) -> suggests epididymitis more than torsion)
Absent cremasteric reflex(elevation of the testis in response to stroking of the upper inner thigh)
(it also may be absent in boys without torsion, particularly if they are younger than six months)
{mem tip: 벌써 올라가있으니까 - 환자의 근육이 올린다}
The testis may be lying horizontally, displacing the epididymis from its normal posterolateral position.
Scrotal swelling/edema
Nausea vomiting
(Nearly 90 percent of patients may have associated nausea and vomiting)
Dx:
-----------------------
Scrotal ultrasound (Collour doppler)
Abnormal urinalysis suggests epididymitis/orchitis more than testicular torsion
Rx:
-----------------------
- Analgesia
- immediate urological consultation for emergency scrotal exploration
Typical rates of viability:
* Detorsion within 4 to 6 hours — 100 percent viability
* Detorsion after 12 hours — 20 percent viability
* Detorsion after 24 hours — 0 percent viability
- if surgery is not available within 6 hours [13] or while preparations for surgery are being made -> manual de-torsion
Manual de-torsion is a temporising measure. The technique involves rotating the right testicle counter-clockwise and the left testicle
clockwise. In other words, the affected testicle is rotated as if opening a book, hence the 'open book' method.
Epididymitis
===================
Symps
--------------
Pain and swelling typically develops over the course of a few days (unlike testicular torsion, which is usually of sudden onset).
The affected testis has a normal vertical lie
Pt may experience pain relief with elevation of the testis (Prehn sign)
Painful micturition (uncommon)
urethral discharge (uncommon)
Epididymitis is caused by organisms causing UTI/STI.
Rx:
--------------
Sexually transmitted:
-cetriaxone 250 mg IMI stat AND
-doxycycline 100 mg BD PO for 14 days
(NOTE: Doxycycline is not approved for use in children younger than the age of eight years)
Not sexually transmitted:
-empiric quinolone: ofloxacin 300 mg BD PO for 10 days OR levofloxacin 500 mg dly PO for 10 days
(NOTE: Fluoroquinolones are not approved for use in patients younger than 18 years of age when other effective alternatives are available)
Prog
--------------
Swelling of testis from epididymitis may takes a month or more to subside
2013년 6월 22일 토요일
Pre-eclampsia
Pre-ecampsia:
Def:
----------------
Hypertension ( sys BP > 140 and/or dia BP > 90 ) with
Proteinuria ( urinary protein > 0.3 g/ 24hr or 1+ protein on urine dipstix )
that develops after 20 wks gestational age.
Classification:
----------------
mild to moderate:
-sys BP 140~160, and/or, dia BP 90~110
severe:
one of the following:
-sys BP > 160, and/or, dia BP > 110
-proteinuria > 5g/24hrs or >= 3+ on urine dipstix
-Oliguria <500 mL/24 hours
-Cerebral or visual disturbances
-Pulmonary oedema or cyanosis
-Epigastric or right upper quadrant pain
-Impaired liver function
-Thrombocytopenia
-Fetal growth restriction.
{간단히보면 BP, proteinuria, HELLP synrome sign, fetus 중에 하나 이상, 요렇게 보자}
Symps/signs:
----------------
Danger signs:
-severe or persistent headache, nausea or vomiting, visual changes(blurry vision)<suggesting cerebral pathology/hemorrhage>,
-shortness of breath<suggesting pulmonary edema>,
-right upper quadrant or epigastric pain <suggesting liver hemorrhage>or
-decreased urine output <suggesting renal failure>
Dx
----------------
do FBC, UE, AST;ALT (to pick up HELLP syndrome : HE(hemolysis - low Hb) L (deranged liver enzyme) LP (low platelete) syndrome)
fetal ultrasound
Mx
----------------
Severe preeclampsia:
Think 4 things: hypertension, seizure, organ dysfunction, fetus
* hypertension -> IV fluid, labetalol/methyldopa
* seizure -> magnesium sulphate
* organdysfunction-> delivery
* fetus-> betamethasone and delivery
{mem tip
(피하시오) -> 피-fetus, 하-hypertension, 시-seizure, 오-organ dysfunction)
Rx 순서: seziure -> HT
씨~~~~이~~ 하!
}
1) prevent/treat seizure:
- Magnesium sulphate: 4 g in 200ml normal saline IVI over 20 mintues + 10 g IM statI
- followed by 5 g IMI every 4 hrs for 24 hrs.
#just good to know:
(MgSO4 has shown benefit in established seizures but its role in prevention of seizures is uncertain.)
#watch out for toxicity:
(progression of clinical pictures in MgSO4 toxicity with increasing MgSO4 serum level:
loss of tendon reflex -> respiratory paralysis -> cardiac arrest )
2) IV maintenance fluid:
- 300 ml R/L IV stat
(if giving magnesium sulphate in 200 ml normal saline, give 100 ml Ringers Lactate instead of 300 ml because the two adds up to be 300 ml in total (200ml NS + 100ml R/L)
- then continue maintenance fluid: 80 mL/hour
3) Treat Hypertension:
-IV Labetalol:
(20 mg - 40 mg - 80 mg - 80 mg (at 10 minute intervals until desired response)
max dose: 220 mg in total.)
#Goal BP: <150 / 100
-Methyldopa 500 mg tds PO
4) Mature the fetal lung:
-Betamethasone 12 mg IM 12 hrly (give total of 2 doses)
5) reverse organ dysfunction
-Deliver the baby
Def:
----------------
Hypertension ( sys BP > 140 and/or dia BP > 90 ) with
Proteinuria ( urinary protein > 0.3 g/ 24hr or 1+ protein on urine dipstix )
that develops after 20 wks gestational age.
Classification:
----------------
mild to moderate:
-sys BP 140~160, and/or, dia BP 90~110
severe:
one of the following:
-sys BP > 160, and/or, dia BP > 110
-proteinuria > 5g/24hrs or >= 3+ on urine dipstix
-Oliguria <500 mL/24 hours
-Cerebral or visual disturbances
-Pulmonary oedema or cyanosis
-Epigastric or right upper quadrant pain
-Impaired liver function
-Thrombocytopenia
-Fetal growth restriction.
{간단히보면 BP, proteinuria, HELLP synrome sign, fetus 중에 하나 이상, 요렇게 보자}
Symps/signs:
----------------
Danger signs:
-severe or persistent headache, nausea or vomiting, visual changes(blurry vision)<suggesting cerebral pathology/hemorrhage>,
-shortness of breath<suggesting pulmonary edema>,
-right upper quadrant or epigastric pain <suggesting liver hemorrhage>or
-decreased urine output <suggesting renal failure>
Dx
----------------
do FBC, UE, AST;ALT (to pick up HELLP syndrome : HE(hemolysis - low Hb) L (deranged liver enzyme) LP (low platelete) syndrome)
fetal ultrasound
Mx
----------------
Severe preeclampsia:
Think 4 things: hypertension, seizure, organ dysfunction, fetus
* hypertension -> IV fluid, labetalol/methyldopa
* seizure -> magnesium sulphate
* organdysfunction-> delivery
* fetus-> betamethasone and delivery
{mem tip
(피하시오) -> 피-fetus, 하-hypertension, 시-seizure, 오-organ dysfunction)
Rx 순서: seziure -> HT
씨~~~~이~~ 하!
}
1) prevent/treat seizure:
- Magnesium sulphate: 4 g in 200ml normal saline IVI over 20 mintues + 10 g IM statI
- followed by 5 g IMI every 4 hrs for 24 hrs.
#just good to know:
(MgSO4 has shown benefit in established seizures but its role in prevention of seizures is uncertain.)
#watch out for toxicity:
(progression of clinical pictures in MgSO4 toxicity with increasing MgSO4 serum level:
loss of tendon reflex -> respiratory paralysis -> cardiac arrest )
2) IV maintenance fluid:
- 300 ml R/L IV stat
(if giving magnesium sulphate in 200 ml normal saline, give 100 ml Ringers Lactate instead of 300 ml because the two adds up to be 300 ml in total (200ml NS + 100ml R/L)
- then continue maintenance fluid: 80 mL/hour
3) Treat Hypertension:
-IV Labetalol:
(20 mg - 40 mg - 80 mg - 80 mg (at 10 minute intervals until desired response)
max dose: 220 mg in total.)
#Goal BP: <150 / 100
-Methyldopa 500 mg tds PO
4) Mature the fetal lung:
-Betamethasone 12 mg IM 12 hrly (give total of 2 doses)
5) reverse organ dysfunction
-Deliver the baby
2013년 6월 20일 목요일
Corticosteroid
Giving corticosteroid
====================
Suppressive action of corticosteroid on cortisol secretion is least when it is given as a SINGLE dose in the MORNING.
(Therefore, give corticosteriod in the morning as a single dose and not at night)
/////////
HPA(hypothalamic-pituitary-adrenal axis) suppression likely ? Patients who have received glucocorticoids who meet the following
criteria are presumed to have HPA suppression:
-Anyone who has received a glucocorticoid dose comparable to more than 20 mg of prednisone a day for more than three weeks.
-Anyone who has received an evening/bedtime dose of prednisone for more than a few weeks.
-Any patient who has a Cushingoid appearance
///////
///////
Tapering regimen
10 mg/day every one to two weeks at an initial dose above 60 mg of prednisone or equivalent per day.
5 mg/day every one to two weeks at prednisone doses between 60 and 20 mg/day.
2.5 mg/day every one to two weeks at prednisone doses between 19 and 10 mg/day.
1 mg/day every one to two weeks at prednisone doses between 9 and 5 mg/day.
0.5 mg/day every one to two weeks at prednisone doses below 5 mg/day. This can be achieved by alternating daily doses, eg, 5
mg on day 1 and 4 mg on day 2. (i.e. 1 mg/ every 2 days)
[..-60-20-10-5-..]
[10-5-2.5-1-0.5]
////////
signs of adrenal insufficiency:
----------------------------
shock
non-specific malaise
side effect of corticosteroid
---------------------------
mem tip: 오잉 (내가 왜) 고혈압에 당뇨지?
-osteoporosis
-infection
-hypertension
-hyperglycemia
====================
Suppressive action of corticosteroid on cortisol secretion is least when it is given as a SINGLE dose in the MORNING.
(Therefore, give corticosteriod in the morning as a single dose and not at night)
/////////
HPA(hypothalamic-pituitary-adrenal axis) suppression likely ? Patients who have received glucocorticoids who meet the following
criteria are presumed to have HPA suppression:
-Anyone who has received a glucocorticoid dose comparable to more than 20 mg of prednisone a day for more than three weeks.
-Anyone who has received an evening/bedtime dose of prednisone for more than a few weeks.
-Any patient who has a Cushingoid appearance
///////
///////
Tapering regimen
10 mg/day every one to two weeks at an initial dose above 60 mg of prednisone or equivalent per day.
5 mg/day every one to two weeks at prednisone doses between 60 and 20 mg/day.
2.5 mg/day every one to two weeks at prednisone doses between 19 and 10 mg/day.
1 mg/day every one to two weeks at prednisone doses between 9 and 5 mg/day.
0.5 mg/day every one to two weeks at prednisone doses below 5 mg/day. This can be achieved by alternating daily doses, eg, 5
mg on day 1 and 4 mg on day 2. (i.e. 1 mg/ every 2 days)
[..-60-20-10-5-..]
[10-5-2.5-1-0.5]
////////
signs of adrenal insufficiency:
----------------------------
shock
non-specific malaise
side effect of corticosteroid
---------------------------
mem tip: 오잉 (내가 왜) 고혈압에 당뇨지?
-osteoporosis
-infection
-hypertension
-hyperglycemia
Bell's palsy
Bell's palsy
=============
Defi:
---------------
idiopathic
sudden onset
unilateral facial nerve paralysis
typically shows some degree of improval within 4 to 6 months.
If known etiology, or If slowly progressive -> not Bell's palsy
Symp
---------------
Motor: Unilateral paralysis (lower motor neuron involving all branches of facial nerve)
Sensory: Facial pain along the course of the facial nerve
Dry eye
Clinical exam
---------------
ipsilateral conductive loss(sensorineural hearing loss) should be invesitaged for possible middle ear infection/neoplastic lesions
Diff Dx
---------------
Stroke - forehead is spared. other neurological dysfunctions are often present.
Middle ear infection complication
Tumour - ipsilateral hearing loss
mem tip: 스튜오(디스 이름이) Bell.
Rx:
---------------
BMJ BEST PRACTICE -> Predisone 25 mg dly PO for 10 days
UPTODATE -> Prednisone 60 mg dly PO for 7 days + valacyclovir 1g tds PO for 7 days
eye protection - artificial tears, ophthalmic lubricant
Prognosis:
---------------
71 % pts recovers to normal or near normal (24 % recovers to normal)
=============
Defi:
---------------
idiopathic
sudden onset
unilateral facial nerve paralysis
typically shows some degree of improval within 4 to 6 months.
If known etiology, or If slowly progressive -> not Bell's palsy
Symp
---------------
Motor: Unilateral paralysis (lower motor neuron involving all branches of facial nerve)
Sensory: Facial pain along the course of the facial nerve
Dry eye
Clinical exam
---------------
ipsilateral conductive loss(sensorineural hearing loss) should be invesitaged for possible middle ear infection/neoplastic lesions
Diff Dx
---------------
Stroke - forehead is spared. other neurological dysfunctions are often present.
Middle ear infection complication
Tumour - ipsilateral hearing loss
mem tip: 스튜오(디스 이름이) Bell.
Rx:
---------------
BMJ BEST PRACTICE -> Predisone 25 mg dly PO for 10 days
UPTODATE -> Prednisone 60 mg dly PO for 7 days + valacyclovir 1g tds PO for 7 days
eye protection - artificial tears, ophthalmic lubricant
Prognosis:
---------------
71 % pts recovers to normal or near normal (24 % recovers to normal)
2013년 6월 17일 월요일
Meniere's disease
Meniere's disease
====================
Meniere's disease - idiopathic {mem tip "D"isease = i"D"iopathic)
Meniere's syndrome - secondary to a cause
Proposed pathogenesis
----------------------
endolymphic hydrops (hydrops: excessive accumulation of serous fluid in tissues or cavities of the body)
Symptoms
--------------------
-Hearing loss (Sensorineural hearing loss is fluctuating and progressive. Vertigo episodes last from 20 minutes to 24 hours, and
typically occur in clusters)
-Tinnitis
-Vertigo (episodic , sudden onset vertigo)
-Sensation of fullness in the affected ear.
-positive Romberg's test (common)
(Swaying or falling when asked to stand with feet together and eyes closed.)
-positive Fukuda's stepping test (common)
(Turning towards the affected side when asked to march in place with eyes closed.)
-inability to walk tandem (heel-to-toe) in a straight line (often)
-Sensorineural hearing loss
Dx
--------------------
Meniere's disease is a clinical diagnosis. Although not diagnostic, patients should undergo audiometry, vestibular testing, and MRI
to rule out other causes of symptoms
Rx:
--------------------
all pt
- low salt diet ( < 1500~2000 mg/day )
- triamterene/hydrochlorothiazide : 50/25 mg orally once daily
or
acetazolamide : 250 mg orally (regular-release) twice daily
symptomatic vetigo
- promethazine: 12.5 to 25 mg orally/rectally every 4-6 hours when required
- <adjunct> intratympanic injections (dexmethasone)
- <adjunct> Meniett device
tinnitis
- tinnitis masker (Tinnitus maskers (white noise generators) are devices similar to hearing aids that fit behind the ear.)
- hearing aids(Hearing aids may help in masking the tinnitus), etc
- if unresponsive to non-pharm Rx: amitriptyline : 25-75 mg/day orally given in 1-3 divided doses
sudden hearing loss
- prednisolone : 20 mg orally three times daily for 2-3 weeks, then gradually taper, or
- Intratympanic corticosteroids
onging symptoms -> surgery
====================
Meniere's disease - idiopathic {mem tip "D"isease = i"D"iopathic)
Meniere's syndrome - secondary to a cause
Proposed pathogenesis
----------------------
endolymphic hydrops (hydrops: excessive accumulation of serous fluid in tissues or cavities of the body)
Symptoms
--------------------
-Hearing loss (Sensorineural hearing loss is fluctuating and progressive. Vertigo episodes last from 20 minutes to 24 hours, and
typically occur in clusters)
-Tinnitis
-Vertigo (episodic , sudden onset vertigo)
-Sensation of fullness in the affected ear.
-positive Romberg's test (common)
(Swaying or falling when asked to stand with feet together and eyes closed.)
-positive Fukuda's stepping test (common)
(Turning towards the affected side when asked to march in place with eyes closed.)
-inability to walk tandem (heel-to-toe) in a straight line (often)
-Sensorineural hearing loss
Dx
--------------------
Meniere's disease is a clinical diagnosis. Although not diagnostic, patients should undergo audiometry, vestibular testing, and MRI
to rule out other causes of symptoms
Rx:
--------------------
all pt
- low salt diet ( < 1500~2000 mg/day )
- triamterene/hydrochlorothiazide : 50/25 mg orally once daily
or
acetazolamide : 250 mg orally (regular-release) twice daily
symptomatic vetigo
- promethazine: 12.5 to 25 mg orally/rectally every 4-6 hours when required
- <adjunct> intratympanic injections (dexmethasone)
- <adjunct> Meniett device
tinnitis
- tinnitis masker (Tinnitus maskers (white noise generators) are devices similar to hearing aids that fit behind the ear.)
- hearing aids(Hearing aids may help in masking the tinnitus), etc
- if unresponsive to non-pharm Rx: amitriptyline : 25-75 mg/day orally given in 1-3 divided doses
sudden hearing loss
- prednisolone : 20 mg orally three times daily for 2-3 weeks, then gradually taper, or
- Intratympanic corticosteroids
onging symptoms -> surgery
2013년 6월 16일 일요일
Hydrocele / Varicocele
Hydrocele
==================
Def:
---------------------
Hydrocele is a collection of serous fluid between the layers of the membrane (tunica vaginalis) that surrounds the testis or along the spermatic cord.
Two Types:
---------------------
1. communicating - processus vaginalis communicates with the peritoneal cavity
2. non-communicating - processus vaginalis does not communicate with the peritoneal cavity, but more fluid is produced by the tunica vaginalis than it is absorbed.
Dx:
---------------------
Clinical diagnosis: transluilluminable, soft(may be tense if small) scrotal mass
If other/additional Dx is suspected ( e.g. with fever, vomitting, diarrhoea, testis not palpable etc ) -> Sonar scrotum
Rx:
---------------------
4 options:
- 1. Observation
- 2. Surgical excision of the hydrocele sac
- 3. Simple aspiration - generally unsuccessful due to rapid reaccumulation of fluid.
- 4. Sclerotherapy
(When fertility is not an issue, aspiration of the hydrocele followed by instillation of sclerosing agent into the scrotum.
Complication:
reactive orchitis/epididymitis and a higher rate of recurrence/makes open surgery more difficult due to adhesion.)
///////////
in children:
<= 2 yr : observation
>= 2 yr : surgery
In adults :
- wihtout discomfort or infection - observation
- with discomfort or infection - surgery or sclerotherapy
//////////
Varicocele
==================
Def:
--------------------
abnormal dilatation of venous pelux
Grade:
--------------------
1. small, palpable only with valsalva
2. moderate, PALPABLE on standing, non-visible
3. large, VISIBLE on gross inspection.
Dx:
--------------------
Ninety percent of varicoceles are on the left side, while approximately 10% are bilateral. A right-sided varicocele alone is rare and should raise suspicion of the presence of a retroperitoneal or pelvic compressive mass.
Scrotal Sonar
'bag of worms' appearance
///////////////
Reason why it occurs on the left commonly:
Left testicular vein drains into left renal vein.
Left renal vein's pressure is higher than testicular vein because it's compressed between aorta and superior mesenteric vein.
This leads to failure of venous valves, causing varicocele.
//////////////
Rx:
--------------------
Warn patient about possible decreased fertility.
If fertility is a concern to the pt -> semen analysis every 2 years.
Young pt (<= 20 yr) with clinically obvious hydrocele -> Surgery
Otherwise observation.
==================
Def:
---------------------
Hydrocele is a collection of serous fluid between the layers of the membrane (tunica vaginalis) that surrounds the testis or along the spermatic cord.
Two Types:
---------------------
1. communicating - processus vaginalis communicates with the peritoneal cavity
2. non-communicating - processus vaginalis does not communicate with the peritoneal cavity, but more fluid is produced by the tunica vaginalis than it is absorbed.
Dx:
---------------------
Clinical diagnosis: transluilluminable, soft(may be tense if small) scrotal mass
If other/additional Dx is suspected ( e.g. with fever, vomitting, diarrhoea, testis not palpable etc ) -> Sonar scrotum
Rx:
---------------------
4 options:
- 1. Observation
- 2. Surgical excision of the hydrocele sac
- 3. Simple aspiration - generally unsuccessful due to rapid reaccumulation of fluid.
- 4. Sclerotherapy
(When fertility is not an issue, aspiration of the hydrocele followed by instillation of sclerosing agent into the scrotum.
Complication:
reactive orchitis/epididymitis and a higher rate of recurrence/makes open surgery more difficult due to adhesion.)
///////////
in children:
<= 2 yr : observation
>= 2 yr : surgery
In adults :
- wihtout discomfort or infection - observation
- with discomfort or infection - surgery or sclerotherapy
//////////
Varicocele
==================
Def:
--------------------
abnormal dilatation of venous pelux
Grade:
--------------------
1. small, palpable only with valsalva
2. moderate, PALPABLE on standing, non-visible
3. large, VISIBLE on gross inspection.
Dx:
--------------------
Ninety percent of varicoceles are on the left side, while approximately 10% are bilateral. A right-sided varicocele alone is rare and should raise suspicion of the presence of a retroperitoneal or pelvic compressive mass.
Scrotal Sonar
'bag of worms' appearance
///////////////
Reason why it occurs on the left commonly:
Left testicular vein drains into left renal vein.
Left renal vein's pressure is higher than testicular vein because it's compressed between aorta and superior mesenteric vein.
This leads to failure of venous valves, causing varicocele.
//////////////
Rx:
--------------------
Warn patient about possible decreased fertility.
If fertility is a concern to the pt -> semen analysis every 2 years.
Young pt (<= 20 yr) with clinically obvious hydrocele -> Surgery
Otherwise observation.
2013년 6월 13일 목요일
Rheumatoid arthritis
- Rheumatoid Arthritis Criteria:
- -------------------------------
- Four of the following:
- 1 : Morning stiffness > 1 hr
- 3 : Affecting more than 3 joints
- <--> : symmetrical
- △
- | : involving hands and feet
- ▽
- (above 4 things for 6 weeks)
- R : Rheumatoid factor positive
- R : Rheumatoid nodules over extensor surfaces
- R : Radiographic changes
BPPV (Benign paroxysmal positional vertigo)
Background Knowledge:
-------------------------------------------------------
Semicircular canal has three components:
anterior(superior), posterior, lateral(horizontal) canal
Posterior canal BPPV — The Dix-Hallpike maneuver
--------------------------------------------------------------
Method:
- The patient's head is turned 45° towards the ear being tested.
- The head is supported, and then the patient is quickly lowered into the supine position with the head extending about 30° below the horizontal while remaining turned 45° towards the ear being tested.
- The head is held in this position and the physician checks for nystagmus.
- To complete the manoeuvre, the patient is returned to a seated position and the eyes are again observed for reversal nystagmus.
Interpretation (Positive Hallpike test):
Head is turned to the right, to test the right ear.
If the right ear is affected, nystagmus occurs as described below:
A: When the head is lowered 30 degree below the bed,
the fast phase of the nystagmus is upward , rotating toward the affected ear
B: When the patient is brought back to the sitting position,
the fast phase of the nystagmus is downward , rotating toward the affected ear
Anterior canal BPPV - The Dix-Hallpike maneuver
--------------------------------------------------------------
Method:
- same as posterior canal BPPV
Interpretation:
In positive Hallpike test, the nystagmus is downbeat and torsional(rotational), with the top of the eye torting away from the lower ear.
Treatment of Posterior or Anterior canal BPPV
--------------------------------------------------------------
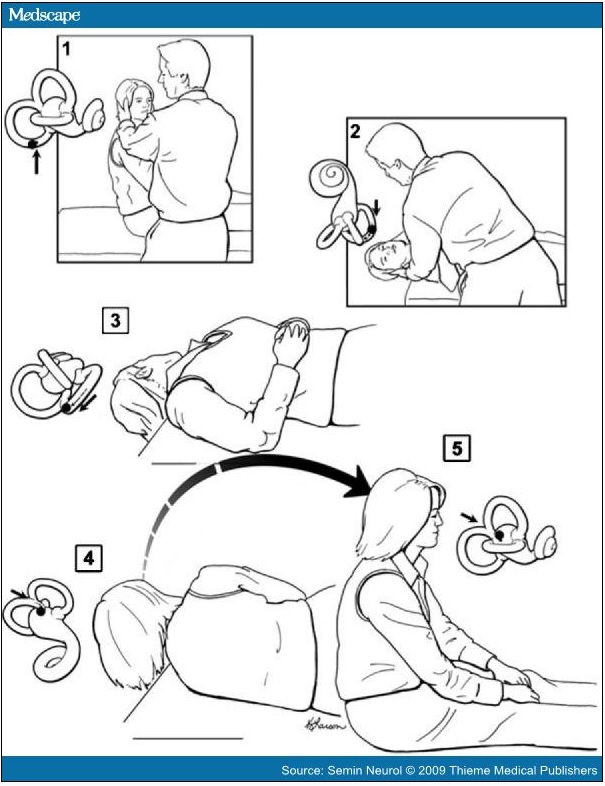
Two methods: Epley maneuver and Semont maneuver
Epley maneuver
/////////////////
Place the patient in a sitting position on the end of the examination table.
Rotate the head 45° towards the affected ear, then swiftly place the patient in a supine position with the head hanging 30° below the horizontal at the end of the examining table (Dix-Hallpike position).
Observe for nystagmus and hold the position for ~30 seconds after it stops.
The head is rotated 90° towards the opposite ear while maintaining the head hanging position.
Observe for nystagmus and hold the position for ~30 seconds after it stops.
Continue then to roll the whole patient another 90° towards the unaffected side until their head is facing 180° from the original Dix-Hallpike position. This change in position should take <3 to 5 seconds.
Observe for nystagmus and hold the position for ~30 seconds after it stops.
Then have the patient sit up. Upon sitting, there should be no vertigo or nystagmus in a successful manoeuvre, because the particles will have been cleared from the posterior semicircular canal back into the utricle.
If there is not paroxysmal nystagmus or symptoms during Dix-Hallpike positioning (Steps 1, 2) then there is a high likelihood of success.
/////////////////
Semont maneuver
////////////////
Sit the patient midway along the long side of an examination table, with their legs hanging over the edge.
Rotate the head 45° towards the unaffected side. While maintaining the head rotation, swiftly place the patient's upper body in a side-lying position on the affected side, with the head resting on the examination table and now facing upwards. This may induce nystagmus and vertigo because of particle movement towards the apex of the semicircular canal. Maintain this position until the vertigo and nystagmus stop (1 to 2 minutes).
Move the patient rapidly through the sitting position of step 1 and into the opposite side-lying position while maintaining the same head rotation, so that the head is resting on the examination table and now facing downwards. A nystagmus response in the same direction would indicate that the particles are exiting the semicircular canal. The transition from step 2 to 3 relies on inertia, and therefore it must be done very quickly. Maintain this position until the vertigo and nystagmus stop (1 to 2 minutes). Slowly return the patient to the sitting position of step 1.
Lateral(Horizontal) canal BPPV - Supine head turn maneuver
--------------------------------------------------------------
The nystagmus of horizontal canal BPPV, unlike that of posterior canal BPPV, is distinctly horizontal(moving to the left and or to the right, i.e. not up and down) and changes direction with changes in head position. There is no torsional(rotational) component.
The paroxysmal direction changing nystagmus may be either geotropic or apogeotropic.
Geotropic direction-changing positional nystagmus is right beating upon turning the head to the right and then left beating when turning the head back to the left side. (geotropic nystagmus = nystagmus "towards ground")
Conversely, the apogeotropic form indicates the nystagmus is right beating with turning to the left and left beating with turning to the right. (apogeotropic nystagmus = nystagmus "away from ground")
In geotropic nystagmus,
The downward ear, on the side where the nystagmus is more intense = the affected ear.
In apogeotrpic nystagmus,
The downward ear, on the side where the nystagmus is less intense = the affected ear.
{그냥 쉽게 병변 쪽으로 nystagmus 가 더 심하게 흘겨 본다고 보면 됨}
The latency is often brief, and the duration may be 15 to 60 seconds. This nystagmus appears less apt to fatigue with repeat
positioning than in cases of posterior canal BPPV; consequently, patients are more likely to become ill with attempts to fatigue this
form of BPPV.
(There is speculation that apogeotropic direction-changing nystagmus suggests cupulolithiasis, and geotropic nystagmus
suggests canalithiasis as the mechanism.)
Treatment of Lateral(Horizontal) canal BPPV
--------------------------------------------------------------
Lempert roll maneuver
////////////////////////
Lempert 360- (Barbeque) degree roll maneuver to treat horizontal canal BPPV. When the patient's head is positioned with the affected ear down, the head is then turned quickly 90 degrees toward the unaffected side (face up). A series of 90-degree turns toward the unaffected side is then undertaken sequentially until the patient has turned 360 degrees and is back to the affected ear-down position. From there, the patient is turned to the face-up position and then brought up to the sitting position. The successive head turns can be done in 15- to 20-second intervals even when the nystagmus continues. Waiting longer does no harm, but may lead to the patient developing nausea, and the shorter interval does not appear to detract from the effectiveness of the treatment.
////////////////////////
Gufoni maneuver
////////////////////////
(1) patient seated on the examination couch with both the legs hanging out from the same side, arms held close to the body, and
hands resting on the knees
(2) patient is then made to lie down on the uninvolved lateral side with a quick lateral movement and maintained in this position for 2
minutes until the end of evoked geotropic nystagmus
(3) quick 45° rotation of the head towards the floor, position being maintained for 2 minutes
(4) slow return back to the starting position
////////////////////////
Chracteristics of BPPV:
---------------------------------
- The latency, transience, and fatigability of the nystagmus
(latency - few seconds (2~5 sec)
transience - usu. lasts less than 30 sec
fatigability - nystagmus / diziness weakens with repeted maneuver)
- Typical mixed upbeat/downbeat + torsional(rotational) nystagmus
Characteristics of Central disorder:
---------------------------------
Latency - none
duration of nystagmus - greater than 1 minute
not-fatiguing
(videos:
Post/Ant canal BPPV
http://www.youtube.com/watch?v=59EIKztATiw
http://www.youtube.com/watch?v=LsPURdtMjac
Laterl canal BPPV
http://www.youtube.com/watch?v=iOJOArGmepM
http://balancemd.net/Horizontal_Canal_BPPV.html)
-------------------------------------------------------
Semicircular canal has three components:
anterior(superior), posterior, lateral(horizontal) canal
Posterior canal BPPV — The Dix-Hallpike maneuver
--------------------------------------------------------------
Method:
- The patient's head is turned 45° towards the ear being tested.
- The head is supported, and then the patient is quickly lowered into the supine position with the head extending about 30° below the horizontal while remaining turned 45° towards the ear being tested.
- The head is held in this position and the physician checks for nystagmus.
- To complete the manoeuvre, the patient is returned to a seated position and the eyes are again observed for reversal nystagmus.
Interpretation (Positive Hallpike test):
Head is turned to the right, to test the right ear.
If the right ear is affected, nystagmus occurs as described below:
A: When the head is lowered 30 degree below the bed,
the fast phase of the nystagmus is upward , rotating toward the affected ear
B: When the patient is brought back to the sitting position,
the fast phase of the nystagmus is downward , rotating toward the affected ear
Anterior canal BPPV - The Dix-Hallpike maneuver
--------------------------------------------------------------
Method:
- same as posterior canal BPPV
Interpretation:
In positive Hallpike test, the nystagmus is downbeat and torsional(rotational), with the top of the eye torting away from the lower ear.
Treatment of Posterior or Anterior canal BPPV
--------------------------------------------------------------
Two methods: Epley maneuver and Semont maneuver
Epley maneuver
/////////////////
Place the patient in a sitting position on the end of the examination table.
Rotate the head 45° towards the affected ear, then swiftly place the patient in a supine position with the head hanging 30° below the horizontal at the end of the examining table (Dix-Hallpike position).
Observe for nystagmus and hold the position for ~30 seconds after it stops.
The head is rotated 90° towards the opposite ear while maintaining the head hanging position.
Observe for nystagmus and hold the position for ~30 seconds after it stops.
Continue then to roll the whole patient another 90° towards the unaffected side until their head is facing 180° from the original Dix-Hallpike position. This change in position should take <3 to 5 seconds.
Observe for nystagmus and hold the position for ~30 seconds after it stops.
Then have the patient sit up. Upon sitting, there should be no vertigo or nystagmus in a successful manoeuvre, because the particles will have been cleared from the posterior semicircular canal back into the utricle.
If there is not paroxysmal nystagmus or symptoms during Dix-Hallpike positioning (Steps 1, 2) then there is a high likelihood of success.
/////////////////
Semont maneuver
////////////////
Sit the patient midway along the long side of an examination table, with their legs hanging over the edge.
Rotate the head 45° towards the unaffected side. While maintaining the head rotation, swiftly place the patient's upper body in a side-lying position on the affected side, with the head resting on the examination table and now facing upwards. This may induce nystagmus and vertigo because of particle movement towards the apex of the semicircular canal. Maintain this position until the vertigo and nystagmus stop (1 to 2 minutes).
Move the patient rapidly through the sitting position of step 1 and into the opposite side-lying position while maintaining the same head rotation, so that the head is resting on the examination table and now facing downwards. A nystagmus response in the same direction would indicate that the particles are exiting the semicircular canal. The transition from step 2 to 3 relies on inertia, and therefore it must be done very quickly. Maintain this position until the vertigo and nystagmus stop (1 to 2 minutes). Slowly return the patient to the sitting position of step 1.
Lateral(Horizontal) canal BPPV - Supine head turn maneuver
--------------------------------------------------------------
The nystagmus of horizontal canal BPPV, unlike that of posterior canal BPPV, is distinctly horizontal(moving to the left and or to the right, i.e. not up and down) and changes direction with changes in head position. There is no torsional(rotational) component.
The paroxysmal direction changing nystagmus may be either geotropic or apogeotropic.
Geotropic direction-changing positional nystagmus is right beating upon turning the head to the right and then left beating when turning the head back to the left side. (geotropic nystagmus = nystagmus "towards ground")
Conversely, the apogeotropic form indicates the nystagmus is right beating with turning to the left and left beating with turning to the right. (apogeotropic nystagmus = nystagmus "away from ground")
In geotropic nystagmus,
The downward ear, on the side where the nystagmus is more intense = the affected ear.
In apogeotrpic nystagmus,
The downward ear, on the side where the nystagmus is less intense = the affected ear.
{그냥 쉽게 병변 쪽으로 nystagmus 가 더 심하게 흘겨 본다고 보면 됨}
The latency is often brief, and the duration may be 15 to 60 seconds. This nystagmus appears less apt to fatigue with repeat
positioning than in cases of posterior canal BPPV; consequently, patients are more likely to become ill with attempts to fatigue this
form of BPPV.
(There is speculation that apogeotropic direction-changing nystagmus suggests cupulolithiasis, and geotropic nystagmus
suggests canalithiasis as the mechanism.)
Treatment of Lateral(Horizontal) canal BPPV
--------------------------------------------------------------
Lempert roll maneuver
////////////////////////
Lempert 360- (Barbeque) degree roll maneuver to treat horizontal canal BPPV. When the patient's head is positioned with the affected ear down, the head is then turned quickly 90 degrees toward the unaffected side (face up). A series of 90-degree turns toward the unaffected side is then undertaken sequentially until the patient has turned 360 degrees and is back to the affected ear-down position. From there, the patient is turned to the face-up position and then brought up to the sitting position. The successive head turns can be done in 15- to 20-second intervals even when the nystagmus continues. Waiting longer does no harm, but may lead to the patient developing nausea, and the shorter interval does not appear to detract from the effectiveness of the treatment.
////////////////////////
Gufoni maneuver
////////////////////////
(1) patient seated on the examination couch with both the legs hanging out from the same side, arms held close to the body, and
hands resting on the knees
(2) patient is then made to lie down on the uninvolved lateral side with a quick lateral movement and maintained in this position for 2
minutes until the end of evoked geotropic nystagmus
(3) quick 45° rotation of the head towards the floor, position being maintained for 2 minutes
(4) slow return back to the starting position
////////////////////////
Chracteristics of BPPV:
---------------------------------
- The latency, transience, and fatigability of the nystagmus
(latency - few seconds (2~5 sec)
transience - usu. lasts less than 30 sec
fatigability - nystagmus / diziness weakens with repeted maneuver)
- Typical mixed upbeat/downbeat + torsional(rotational) nystagmus
Characteristics of Central disorder:
---------------------------------
Latency - none
duration of nystagmus - greater than 1 minute
not-fatiguing
(videos:
Post/Ant canal BPPV
http://www.youtube.com/watch?v=59EIKztATiw
http://www.youtube.com/watch?v=LsPURdtMjac
Laterl canal BPPV
http://www.youtube.com/watch?v=iOJOArGmepM
http://balancemd.net/Horizontal_Canal_BPPV.html)
2013년 6월 11일 화요일
CXR - Dilated heart

Enlarged globular cardiac silhouette with cardiothoracic ratio of 58%. Right cardiac border forms a double contour; this usually suggests left atrial dilatation, but in this case it is caused by right atrial dilatation.
(reference: Circulation August 26, 2008 vol. 118 no. 9 e133-e135)
Subclinical Hyperthryoidism
Low TSH + Normal FT4 + Normal FT3 -> subclinical hyperthryoidism
studies lack, but hyperthyroidism treatment (antithyroid meds/radioactive iodine) probably helps against osteoporosis and cardiac arrhythmia.
Cause:
Exogenous - thyroid hormone tablet.
Endogenous - multinodular goiter, thyroid adenoma - are the most common cause of endogenous subclinical hyperthyroidism.
Rx:
TSH < 0.1 mU/ml -> treat the cause.
TSH 0.1~0.5
-> in elderly or high risk pt - treat the cause.
-> in low risk pt - observe. repeat blood test every 6 months.
studies lack, but hyperthyroidism treatment (antithyroid meds/radioactive iodine) probably helps against osteoporosis and cardiac arrhythmia.
Cause:
Exogenous - thyroid hormone tablet.
Endogenous - multinodular goiter, thyroid adenoma - are the most common cause of endogenous subclinical hyperthyroidism.
Rx:
TSH < 0.1 mU/ml -> treat the cause.
TSH 0.1~0.5
-> in elderly or high risk pt - treat the cause.
-> in low risk pt - observe. repeat blood test every 6 months.
UA/ Non-STEMI
Angina is considered to be unstable if it is prolonged (lasting more than 20 minutes), if it occurs at rest.
Unstable angina:
absence of biochemical evidence of myocardial damage
clinical findings of prolonged (>20 minutes) angina at rest
NSTEMI is distinguished from UA by the presence of elevated serum biomarkers. ST segment elevations and Q waves are absent in
both UA and NSTEMI. As a result, UA and NSTEMI are frequently indistinguishable at initial evaluation since an elevation in serum
biomarkers is usually not detectable for four to six hours after an MI, and at least 12 hours are required to detect elevations in all
patients.
DX:
----------
Cardiac biomarkers (troponin I or T, and creatine kinase-MB [CK-MB]) should be measured on presentation.
CK-MB has low sensitivity during early (<6 hours) or late (>36 hour) symptom onset and for minor damage.
CK-MB also has low specificity
Both troponin T (TnT) and troponin I (TnI) are more specific but have lower sensitivity for the very early detection of myocardial
necrosis. If the early (<6 hours from symptom onset) troponin test is normal, it should be repeated after 8 to 12 hours.
Troponin remains elevated up to 10 to 14 days after release.
ECG findings in UA/NSTEMI: normal or ST depression +- T wave inversion
A repeat ECG should be performed at 6 and 24 hours and if clinical status changes.
{즉,
Normal ECG -> repeat after 8 hrs.
Normal CK-MB, Trop I -> repeat after 8 hrs.
}
RX:
-----------
{
MONA
BS
invasive approach or non-invasive approach
}
MONA (aspirin 300 mg + clopidogrel 300 mg)
(antiplatelet continuation dose - aspirin 75 mg + clopidogrel 75 mg daily PO)
exclude use of errectile drugs (e.g.viagra) before using nitrate.
B(beta blocker) S(statin)
Invasive approach:
-PCI/CABG plus abciximab IVI
Non-invasive approach:
-Enoxaparin sodium 1 mg/kg SC 12hrly X 7 days plus abciximab IVI
An aggressive approach to reperfusion using PCI is best suited for patients with an elevated troponin level or a TIMI risk score ≥5 or
possibly other high-risk features. (See 'High-risk patient' below.) For patients at lower risk, approaches vary based upon hospital
protocol.
Fibrinolytic therapy is not beneficial in patients with a non-ST elevation ACS. (-> This is the difference between STEMI and Non-
STEMI) Therefore, thrombolytic therapy should NOT be administered to patients with UA or NSTEMI unless subsequent ECG
monitoring documents ST segment elevations that persist.
Unstable angina:
absence of biochemical evidence of myocardial damage
clinical findings of prolonged (>20 minutes) angina at rest
NSTEMI is distinguished from UA by the presence of elevated serum biomarkers. ST segment elevations and Q waves are absent in
both UA and NSTEMI. As a result, UA and NSTEMI are frequently indistinguishable at initial evaluation since an elevation in serum
biomarkers is usually not detectable for four to six hours after an MI, and at least 12 hours are required to detect elevations in all
patients.
DX:
----------
Cardiac biomarkers (troponin I or T, and creatine kinase-MB [CK-MB]) should be measured on presentation.
CK-MB has low sensitivity during early (<6 hours) or late (>36 hour) symptom onset and for minor damage.
CK-MB also has low specificity
Both troponin T (TnT) and troponin I (TnI) are more specific but have lower sensitivity for the very early detection of myocardial
necrosis. If the early (<6 hours from symptom onset) troponin test is normal, it should be repeated after 8 to 12 hours.
Troponin remains elevated up to 10 to 14 days after release.
ECG findings in UA/NSTEMI: normal or ST depression +- T wave inversion
A repeat ECG should be performed at 6 and 24 hours and if clinical status changes.
{즉,
Normal ECG -> repeat after 8 hrs.
Normal CK-MB, Trop I -> repeat after 8 hrs.
}
RX:
-----------
{
MONA
BS
invasive approach or non-invasive approach
}
MONA (aspirin 300 mg + clopidogrel 300 mg)
(antiplatelet continuation dose - aspirin 75 mg + clopidogrel 75 mg daily PO)
exclude use of errectile drugs (e.g.viagra) before using nitrate.
B(beta blocker) S(statin)
Invasive approach:
-PCI/CABG plus abciximab IVI
Non-invasive approach:
-Enoxaparin sodium 1 mg/kg SC 12hrly X 7 days plus abciximab IVI
An aggressive approach to reperfusion using PCI is best suited for patients with an elevated troponin level or a TIMI risk score ≥5 or
possibly other high-risk features. (See 'High-risk patient' below.) For patients at lower risk, approaches vary based upon hospital
protocol.
Fibrinolytic therapy is not beneficial in patients with a non-ST elevation ACS. (-> This is the difference between STEMI and Non-
STEMI) Therefore, thrombolytic therapy should NOT be administered to patients with UA or NSTEMI unless subsequent ECG
monitoring documents ST segment elevations that persist.
2013년 6월 8일 토요일
Asthma
=================
Asthma
=================
Symp:
SOB (in)
cough (물 out)
wheeze (공기 out)
inability to speak (소리 out)
Tests:
PEFR
Sats
+- ABG / CXR
Criteria:
mild: PEFR > 70% - dyspnoea only with exertion
moderate: PEFR 40~70 % - dyspnoea limits daily activity
severe: < 40 % - interferes conversation
(peadiatric crteria
PEFR is the same.
mild: talks in sentences
moderate: talks in phrases
severe: talks in words/ can't talk
)
Sat < 90 %
-> at least severe to life threatening asthma
Rx:
Oxygen
Inhaled Short-acting Beta2 agonists
Oral corticosteroid
Inhaled Anticholinergic
Magnesium
{데이빗 "배컴"
BACOM - Beta agonist, Anticholinergic, Corticosteroid, Magnesium
AA - Adrenaline, Antibiotics (adjuntive therapies)
}
///////
--mild--
-Salbutamol 2.5 ~ 5 mg nebulized every 20 min X 3
-Oral corticosteroid - prednisone 40 ~ 80 mg / day X 7 days
(
Pead dose:
Oral corticosteroid - prednisone 1mg/kg/day (max 40mg) (IV dose is the same)
)
--moderate to severe--
-Ipratropium bromide 0.5 mg nebulized in combination with salbutamol as above (every 20 min X 3)
-MgSO4 - 2 g IV over 20 min
---Life threatening ---
-IV hydrocortisone mg IVI 8 hrs (can be switched to oral as soon as possible)
-adjunct -
epinephrine: 0.01 mg/kg IMI as a single dose, if anaphylaxis suspected
antibiotics if infection suspected ( mycoplasma penumonia most common - erythromycin 50mg/kg/day in 4 divided doses)
///////
==================
Asthma
==================
criteria:
mild:
-FEV1 > 80 %
-symptom <= 2 per wk
-night symptom <= 2 per month
(mem tip 2, 2)
moderate:
-FEV1 60~80 %
-symptom daily
-night symptom > 1 per wk
(mem tip 1, 1)
severe:
-FEV1 < 60 %
DX:
Low in both FEV1/FVC and FEV1.
( FEV1/FVC < 80 % predicted
FEV1 < 80 % predicted )
FEV1 improves by 200 ml AND 12 % after bronchodilator.
Rx:
mild - short acting beta agnoist (e.g. salbutamol)
persistent mild - short acting beta agonist + corticosteroid inhaler
moderate - short acting beta agonist + corticosteroid inhaler + long acting beta agonist (e.g. salmeterol)
severe - short acting beta agonist + corticosteroid inhaler + long acting beta agonist (e.g. salmeterol) + oral corticosteroid
Asthma
=================
Symp:
SOB (in)
cough (물 out)
wheeze (공기 out)
inability to speak (소리 out)
Tests:
PEFR
Sats
+- ABG / CXR
Criteria:
mild: PEFR > 70% - dyspnoea only with exertion
moderate: PEFR 40~70 % - dyspnoea limits daily activity
severe: < 40 % - interferes conversation
(peadiatric crteria
PEFR is the same.
mild: talks in sentences
moderate: talks in phrases
severe: talks in words/ can't talk
)
Sat < 90 %
-> at least severe to life threatening asthma
Rx:
Oxygen
Inhaled Short-acting Beta2 agonists
Oral corticosteroid
Inhaled Anticholinergic
Magnesium
{데이빗 "배컴"
BACOM - Beta agonist, Anticholinergic, Corticosteroid, Magnesium
AA - Adrenaline, Antibiotics (adjuntive therapies)
}
///////
--mild--
-Salbutamol 2.5 ~ 5 mg nebulized every 20 min X 3
-Oral corticosteroid - prednisone 40 ~ 80 mg / day X 7 days
(
Pead dose:
Oral corticosteroid - prednisone 1mg/kg/day (max 40mg) (IV dose is the same)
)
--moderate to severe--
-Ipratropium bromide 0.5 mg nebulized in combination with salbutamol as above (every 20 min X 3)
-MgSO4 - 2 g IV over 20 min
---Life threatening ---
-IV hydrocortisone mg IVI 8 hrs (can be switched to oral as soon as possible)
-adjunct -
epinephrine: 0.01 mg/kg IMI as a single dose, if anaphylaxis suspected
antibiotics if infection suspected ( mycoplasma penumonia most common - erythromycin 50mg/kg/day in 4 divided doses)
///////
==================
Asthma
==================
criteria:
mild:
-FEV1 > 80 %
-symptom <= 2 per wk
-night symptom <= 2 per month
(mem tip 2, 2)
moderate:
-FEV1 60~80 %
-symptom daily
-night symptom > 1 per wk
(mem tip 1, 1)
severe:
-FEV1 < 60 %
DX:
Low in both FEV1/FVC and FEV1.
( FEV1/FVC < 80 % predicted
FEV1 < 80 % predicted )
FEV1 improves by 200 ml AND 12 % after bronchodilator.
Rx:
mild - short acting beta agnoist (e.g. salbutamol)
persistent mild - short acting beta agonist + corticosteroid inhaler
moderate - short acting beta agonist + corticosteroid inhaler + long acting beta agonist (e.g. salmeterol)
severe - short acting beta agonist + corticosteroid inhaler + long acting beta agonist (e.g. salmeterol) + oral corticosteroid
Carpal tunnel
Carpal tunnel syndrome
:Compression of median nerve
Symptoms:
{
Sensory - too little (numbness)
- too much (tingling, pain)
Motor - weakness, clumsiness
}
Numbness (thenar eminence is spared - supplied by palmar branch which lies outside the carpal tunnel)
Tingling
Pain (in Hand and arm. Pain may radiate from ventral aspect of wrist proximally to forearm and upper arm. Maybe worse at night)
Clumsiness
Weakness of hand
Tests:
EMG
U/S wrist
MRI wrist
Differential:
c6, c7 radiculopathy
brachial plexopathy
Rx:
Splint
NSAIDs
Corticosteroid injection
Surgical release
:Compression of median nerve
Symptoms:
{
Sensory - too little (numbness)
- too much (tingling, pain)
Motor - weakness, clumsiness
}
Numbness (thenar eminence is spared - supplied by palmar branch which lies outside the carpal tunnel)
Tingling
Pain (in Hand and arm. Pain may radiate from ventral aspect of wrist proximally to forearm and upper arm. Maybe worse at night)
Clumsiness
Weakness of hand
Tests:
EMG
U/S wrist
MRI wrist
Differential:
c6, c7 radiculopathy
brachial plexopathy
Rx:
Splint
NSAIDs
Corticosteroid injection
Surgical release
Dementia
Dementia
majority of cases of dementia are caused by :
1.degenerative causes and by
2.vascular causes
Degenerative causes include Alzheimer's disease (the most common cause of dementia accounting for an estimated 60% of
cases), Parkinson's disease, etc.
Note: 10% to 20% of dementias are caused by potentially reversible conditions
(e.g. infections, inflammatory diseases, neoplasm, toxic insults, metabolic disorders, and trauma )
NB Differential - Delirium is an acute (hours to days), usually reversible, metabolically induced state of fluctuating consciousness.
Adjunct Therapy - antipsychotic (controversial) - haloperidol 0.5 mg bd PO
Behavioural management
-consider stopping all benzo & antipsychotic ( paradoxical aggrevation )
-Mood stabilizer: carbamazepine 100 mg bd po
-lorazepam 0.5 mg PO/IMI when required,
majority of cases of dementia are caused by :
1.degenerative causes and by
2.vascular causes
Degenerative causes include Alzheimer's disease (the most common cause of dementia accounting for an estimated 60% of
cases), Parkinson's disease, etc.
Note: 10% to 20% of dementias are caused by potentially reversible conditions
(e.g. infections, inflammatory diseases, neoplasm, toxic insults, metabolic disorders, and trauma )
NB Differential - Delirium is an acute (hours to days), usually reversible, metabolically induced state of fluctuating consciousness.
Adjunct Therapy - antipsychotic (controversial) - haloperidol 0.5 mg bd PO
Behavioural management
-consider stopping all benzo & antipsychotic ( paradoxical aggrevation )
-Mood stabilizer: carbamazepine 100 mg bd po
-lorazepam 0.5 mg PO/IMI when required,
2013년 6월 4일 화요일
Organophosphate poisoning
Organophosphate poisoning
-Acetylcholine esterase inhibitor -> inc Ach level at the synapses
Signs/Symps:
-increased secretions: lacrimation, salivation, pulmonary edema -> crepitation
-bronchospasm -> wheeze
-pinpoint pupils
-decreased level of consciousness
Dx:
-Atropine trial: poisoned pt show little/no anticholinergic effect. (Look at heart rate (inc), skin dryness, pupil dilatation)
-plasma cholinesterase measurement
-others: ecg, bld gas, CXR
Rx:
- Resus + supportive care: IV + airway + ventilation
- Decontamination ( discard clothes, wash skin, stomach contents aspirated if airway is protected )
- Atropine:
(atropine : 2 mg intravenously initially, followed by double doses (e.g., 4 mg, 8 mg, 16 mg, etc.) every 5 minutes until secretions are controlled. Atropine requirements are extremely variable; daily doses range between 10 and 1000 mg or more.)
{간단히
눈 - constricted pupil, lacrimation
입 - salivation
폐 - pulmonary edema (crepitation), bronchospalsm ( wheeze )
심장 - bradycardia}
-Acetylcholine esterase inhibitor -> inc Ach level at the synapses
Signs/Symps:
-increased secretions: lacrimation, salivation, pulmonary edema -> crepitation
-bronchospasm -> wheeze
-pinpoint pupils
-decreased level of consciousness
Dx:
-Atropine trial: poisoned pt show little/no anticholinergic effect. (Look at heart rate (inc), skin dryness, pupil dilatation)
-plasma cholinesterase measurement
-others: ecg, bld gas, CXR
Rx:
- Resus + supportive care: IV + airway + ventilation
- Decontamination ( discard clothes, wash skin, stomach contents aspirated if airway is protected )
- Atropine:
(atropine : 2 mg intravenously initially, followed by double doses (e.g., 4 mg, 8 mg, 16 mg, etc.) every 5 minutes until secretions are controlled. Atropine requirements are extremely variable; daily doses range between 10 and 1000 mg or more.)
{간단히
눈 - constricted pupil, lacrimation
입 - salivation
폐 - pulmonary edema (crepitation), bronchospalsm ( wheeze )
심장 - bradycardia}
Paed Hx Taking
Paed Hx Taking
-Coughing
-Vomiting
-Diarrhoea
-Feeding
-Fever
-Birth
-Vaccine
-Growth
-HIV
-TB
-Coughing
-Vomiting
-Diarrhoea
-Feeding
-Fever
-Birth
-Vaccine
-Growth
-HIV
-TB
Burn wound / Stevens-Johnson
============================
Burn
============================
classification:
1st degree
-involves epidermis
-red, painful, dry
-blanch with pressure
2nd degree
-involves epidermis + dermis
-red, painful, wet
- (+-)blisters
-blanches with pressure
3rd degree
-involves epidermis + dermis + skin appendages
-white/black, insensate, dry
-does not blanch with pressure
4th degree
-involves epidermis + dermis + skin appendages + subcutaneous tissue / tendon / bone
-white/black, insensate, dry
-does not blanch with pressure
{mem tip:
pain / blanch/ colour / dry-wet
p b c d
}
indication for admission:
-partial-thickness burns of >10% TBSA;
-face, hands, feet, genitalia, perineum, or major joints;
-electrical burns, including lightning injury;
-chemical burns;
-inhalation injury;
-burn injury in patients with pre-existing medical disorders
Rx:
topical antibiotic prophylaxis
(Silver is an excellent antiseptic and is used in burn wound care
The silver helps to prevent infection and remains active for 3 to 4 days, allowing less frequent dressing changes.)
tetanus immunisation
morphine 10 to 30 mg orally every 3-4 hours when required
Fluid resuscitation:
If burns involve >15% of the body surface, loss of capillary integrity becomes significant, requirng fluid resuscitation.
Parkland formula is often used and suggests 4 mL/kg/% burn over the first 24 hours, half in the first 8 hours, generally as lactated
Ringer's solution. Capillary integrity is typically restored at approximately 24 hours.
(Young children should receive 5% dextrose in lactated Ringer's solution (D5LR) at a maintenance rate to ensure that they do not
develop hypoglycaemia.)
infected wound -> debridement + antibiotic
circumferential burns -> escharotomy
Nutrition / physio / occupational therapy
[dose: midazolam : 0.04 mg/kg IVI
morphine: 0.1 mg/kg IVI]
{Burn description 간략히
-깊이
-넓이
-어디
-EIC (에 이 씨) - electrical ( myoglobin inc -> renal impairment, hyperkalemia -> arrhythmia), inhalational burn, chemical // open fire,
boiling water...
}
{Burn Rx 간략히
-Fluid
-Analgesic
-Antibiotic
-Dressing (Silver dressing)
-escharotomy
}
============================
Steven-Johnson syndrome
============================
Rx:
Stop offending agent ( common causative agent: sulfonamide (bactrim), NSAIDS (therefore NSAIDs should not be used for analgesic
unless other medicines, such as opioids or paracetamol, do not work), corticosteroids, etc)
ABC (airway edema -> obstruction)
Dressing (silver dressing (e.g. silver sulfadizine) )
Analgesic (avoid NSAIDs)
Fluid (Parkland formula)
Nutrition / physio / occupational therapy
morphine sulphate : children: 0.1 mg/kg orally/intravenously every 2-4 hours when required, maximum 15 mg/kg;
adults: 7.5-10 mg orally/intravenously every 4 hours when required
adjunct:
1) glucocorticoids
advese effect: may increase risk of infection - infection is the main reason for mortality
use: it can be used in - Adults with burn (%) less than 30 %. Don't use in paed pt, or burn > 30 %.
prednisone 2 mg/kg/day not more than 7 days ( or equivalent amount of prednisolone or methylprednisolone )
2) IV immunoglobulin
Burn
============================
classification:
1st degree
-involves epidermis
-red, painful, dry
-blanch with pressure
2nd degree
-involves epidermis + dermis
-red, painful, wet
- (+-)blisters
-blanches with pressure
3rd degree
-involves epidermis + dermis + skin appendages
-white/black, insensate, dry
-does not blanch with pressure
4th degree
-involves epidermis + dermis + skin appendages + subcutaneous tissue / tendon / bone
-white/black, insensate, dry
-does not blanch with pressure
{mem tip:
pain / blanch/ colour / dry-wet
p b c d
}
indication for admission:
-partial-thickness burns of >10% TBSA;
-face, hands, feet, genitalia, perineum, or major joints;
-electrical burns, including lightning injury;
-chemical burns;
-inhalation injury;
-burn injury in patients with pre-existing medical disorders
Rx:
topical antibiotic prophylaxis
(Silver is an excellent antiseptic and is used in burn wound care
The silver helps to prevent infection and remains active for 3 to 4 days, allowing less frequent dressing changes.)
tetanus immunisation
morphine 10 to 30 mg orally every 3-4 hours when required
Fluid resuscitation:
If burns involve >15% of the body surface, loss of capillary integrity becomes significant, requirng fluid resuscitation.
Parkland formula is often used and suggests 4 mL/kg/% burn over the first 24 hours, half in the first 8 hours, generally as lactated
Ringer's solution. Capillary integrity is typically restored at approximately 24 hours.
(Young children should receive 5% dextrose in lactated Ringer's solution (D5LR) at a maintenance rate to ensure that they do not
develop hypoglycaemia.)
infected wound -> debridement + antibiotic
circumferential burns -> escharotomy
Nutrition / physio / occupational therapy
[dose: midazolam : 0.04 mg/kg IVI
morphine: 0.1 mg/kg IVI]
{Burn description 간략히
-깊이
-넓이
-어디
-EIC (에 이 씨) - electrical ( myoglobin inc -> renal impairment, hyperkalemia -> arrhythmia), inhalational burn, chemical // open fire,
boiling water...
}
{Burn Rx 간략히
-Fluid
-Analgesic
-Antibiotic
-Dressing (Silver dressing)
-escharotomy
}
============================
Steven-Johnson syndrome
============================
Rx:
Stop offending agent ( common causative agent: sulfonamide (bactrim), NSAIDS (therefore NSAIDs should not be used for analgesic
unless other medicines, such as opioids or paracetamol, do not work), corticosteroids, etc)
ABC (airway edema -> obstruction)
Dressing (silver dressing (e.g. silver sulfadizine) )
Analgesic (avoid NSAIDs)
Fluid (Parkland formula)
Nutrition / physio / occupational therapy
morphine sulphate : children: 0.1 mg/kg orally/intravenously every 2-4 hours when required, maximum 15 mg/kg;
adults: 7.5-10 mg orally/intravenously every 4 hours when required
adjunct:
1) glucocorticoids
advese effect: may increase risk of infection - infection is the main reason for mortality
use: it can be used in - Adults with burn (%) less than 30 %. Don't use in paed pt, or burn > 30 %.
prednisone 2 mg/kg/day not more than 7 days ( or equivalent amount of prednisolone or methylprednisolone )
2) IV immunoglobulin
2013년 6월 3일 월요일
Hepatitis B
Hep B e Ag > 3 months
-> high likelihood of chronic infection
Hep B e Ag positive
-> majority have active infection
-> it also indicates greater infectivity.
Hep B core Ab
-> indicates exposure to hepatitis B virus
Hep B surface Ag > 6 months
-> indicates chronic hepatitis B infection
Hep B DNA Qualitative assay
Window period:
[ HBsAg: neg, HBsAb: neg, HBcAb: pos]
The disappearance of HBsAg (hepatitis B surface antigen) is followed by the appearance of anti-HBs. In some patients, however,
anti-HBs may not be detectable until after a window period of several weeks to months. At this time, neither HBsAg nor anti-HBs can
be detected, the serologic diagnosis may be made by the detection of IgM antibodies against hepatitis B core antigen (IgM anti-
HBc).
Rx:
Acute Hep B - fulminant infection:
- supportive
- lamivudine +- liver transplant
Chronic
-interferon
-antiviral therapy (tenofovir, lamivudine, etc)
indication for Rx in chronic infection:
-co-infection with HIV or Hep D
-cirrhosis
-if no coinection/comorbidity:
-HBeAg positive, HBV DNA > 20 000 IU, ALT > twice upper normal limit
-HBeAg negative, HBV dNA > 2 000 IU, ALT > upper normal limit
-> high likelihood of chronic infection
Hep B e Ag positive
-> majority have active infection
-> it also indicates greater infectivity.
Hep B core Ab
-> indicates exposure to hepatitis B virus
Hep B surface Ag > 6 months
-> indicates chronic hepatitis B infection
Hep B DNA Qualitative assay
Window period:
[ HBsAg: neg, HBsAb: neg, HBcAb: pos]
The disappearance of HBsAg (hepatitis B surface antigen) is followed by the appearance of anti-HBs. In some patients, however,
anti-HBs may not be detectable until after a window period of several weeks to months. At this time, neither HBsAg nor anti-HBs can
be detected, the serologic diagnosis may be made by the detection of IgM antibodies against hepatitis B core antigen (IgM anti-
HBc).
Rx:
Acute Hep B - fulminant infection:
- supportive
- lamivudine +- liver transplant
Chronic
-interferon
-antiviral therapy (tenofovir, lamivudine, etc)
indication for Rx in chronic infection:
-co-infection with HIV or Hep D
-cirrhosis
-if no coinection/comorbidity:
-HBeAg positive, HBV DNA > 20 000 IU, ALT > twice upper normal limit
-HBeAg negative, HBV dNA > 2 000 IU, ALT > upper normal limit
Haemorrhoids
Causes of haemorrhoids:
-------------------------
The primary aetiology is believed to be excessive straining due to either chronic constipation or diarrhoea.
Other causes:an increase in intra-abdominal pressure can be caused by pregnancy or ascites;
the presence of space-occupying lesions within the pelvis
Types of haemorrhoids:
-------------------------
1) External haemorrhoids
:Haemorrhoids that are located in the distal anal canal, distal to the dentate line, and covered by sensate anoderm or skin.
2) Internal haemorrhoids
:Haemorrhoids that originate proximal to the dentate line and covered by insensate transitional epithelium
Grade 1 - protrusion is limited to within the anal canal.
Grade 2 - protrudes beyond the anal canal but spontaneously reduces on cessation of straining.
Grade 3 - protrudes outside the anal canal and reduces fully on manual pressure.
Grade 4 - protrudes outside the anal canal and is irreducible.
This grading of internal haemorrhoids is only a reflection of the degree of prolapse but is not a measure of either the disease severity or of the size of haemorrhoidal prolapse.
Rx:
--------------------------
For all grades:
Straining or spending excessive time at stool should be discouraged.
Constipation can be avoided by adding fibre and fluids to the diet; consuming 25 to 30 g of fibre daily .
(+- stool softeners short-term)
grade 1 haemorrhoids
Creams and ointments are generally used for external haemorrhoids
and suppositories are generally used for internal haemorrhoids
hydrocortisone rectal :
(1 to 2.5%) apply twice daily for a maximum of 5-7 days;
25 mg (1 suppository) into the rectum twice daily for 14 days
grade 2
rubber band ligation or sclerotherapy or infrared photocoagulation or haemorrhoid arterial ligation or stapled haemorrhoidopexy
grade 3
rubber band ligation
grade 4
Surgical haemorrhoidectomy
Thrombosed haemorrhoid:
Treatment of acute thrombosis of internal hemorrhoids is usually conservative.
In thrombosed external hemorrhoids, surgical evacuation of the hemorrhoid with excision of the skin overlying the thrombosed hemorrhoid can produce immediate relief. As an alternative, oral and topical analgesics, stool softeners, and sitz baths may provide adequate relief until spontaneous resolution occurs
{간략히
똥
stool softener
누기
don't strain
dietary fiber
아파
topical analgesic
grade I : corticosteroid cream / suppository
> grade I: band ligation / haemorrhoidectomy
}
-------------------------
The primary aetiology is believed to be excessive straining due to either chronic constipation or diarrhoea.
Other causes:an increase in intra-abdominal pressure can be caused by pregnancy or ascites;
the presence of space-occupying lesions within the pelvis
Types of haemorrhoids:
-------------------------
1) External haemorrhoids
:Haemorrhoids that are located in the distal anal canal, distal to the dentate line, and covered by sensate anoderm or skin.
2) Internal haemorrhoids
:Haemorrhoids that originate proximal to the dentate line and covered by insensate transitional epithelium
Grade 1 - protrusion is limited to within the anal canal.
Grade 2 - protrudes beyond the anal canal but spontaneously reduces on cessation of straining.
Grade 3 - protrudes outside the anal canal and reduces fully on manual pressure.
Grade 4 - protrudes outside the anal canal and is irreducible.
This grading of internal haemorrhoids is only a reflection of the degree of prolapse but is not a measure of either the disease severity or of the size of haemorrhoidal prolapse.
Rx:
--------------------------
For all grades:
Straining or spending excessive time at stool should be discouraged.
Constipation can be avoided by adding fibre and fluids to the diet; consuming 25 to 30 g of fibre daily .
(+- stool softeners short-term)
grade 1 haemorrhoids
Creams and ointments are generally used for external haemorrhoids
and suppositories are generally used for internal haemorrhoids
hydrocortisone rectal :
(1 to 2.5%) apply twice daily for a maximum of 5-7 days;
25 mg (1 suppository) into the rectum twice daily for 14 days
grade 2
rubber band ligation or sclerotherapy or infrared photocoagulation or haemorrhoid arterial ligation or stapled haemorrhoidopexy
grade 3
rubber band ligation
grade 4
Surgical haemorrhoidectomy
Thrombosed haemorrhoid:
Treatment of acute thrombosis of internal hemorrhoids is usually conservative.
In thrombosed external hemorrhoids, surgical evacuation of the hemorrhoid with excision of the skin overlying the thrombosed hemorrhoid can produce immediate relief. As an alternative, oral and topical analgesics, stool softeners, and sitz baths may provide adequate relief until spontaneous resolution occurs
{간략히
똥
stool softener
누기
don't strain
dietary fiber
아파
topical analgesic
grade I : corticosteroid cream / suppository
> grade I: band ligation / haemorrhoidectomy
}
피드 구독하기:
글 (Atom)