Hydrocele
==================
Def:
---------------------
Hydrocele is a collection of serous fluid between the layers of the membrane (tunica vaginalis) that surrounds the testis or along the spermatic cord.
Two Types:
---------------------
1. communicating - processus vaginalis communicates with the peritoneal cavity
2. non-communicating - processus vaginalis does not communicate with the peritoneal cavity, but more fluid is produced by the tunica vaginalis than it is absorbed.
Dx:
---------------------
Clinical diagnosis: transluilluminable, soft(may be tense if small) scrotal mass
If other/additional Dx is suspected ( e.g. with fever, vomitting, diarrhoea, testis not palpable etc ) -> Sonar scrotum
Rx:
---------------------
4 options:
- 1. Observation
- 2. Surgical excision of the hydrocele sac
- 3. Simple aspiration - generally unsuccessful due to rapid reaccumulation of fluid.
- 4. Sclerotherapy
(When fertility is not an issue, aspiration of the hydrocele followed by instillation of sclerosing agent into the scrotum.
Complication:
reactive orchitis/epididymitis and a higher rate of recurrence/makes open surgery more difficult due to adhesion.)
///////////
in children:
<= 2 yr : observation
>= 2 yr : surgery
In adults :
- wihtout discomfort or infection - observation
- with discomfort or infection - surgery or sclerotherapy
//////////
Varicocele
==================
Def:
--------------------
abnormal dilatation of venous pelux
Grade:
--------------------
1. small, palpable only with valsalva
2. moderate, PALPABLE on standing, non-visible
3. large, VISIBLE on gross inspection.
Dx:
--------------------
Ninety percent of varicoceles are on the left side, while approximately 10% are bilateral. A right-sided varicocele alone is rare and should raise suspicion of the presence of a retroperitoneal or pelvic compressive mass.
Scrotal Sonar
'bag of worms' appearance
///////////////
Reason why it occurs on the left commonly:
Left testicular vein drains into left renal vein.
Left renal vein's pressure is higher than testicular vein because it's compressed between aorta and superior mesenteric vein.
This leads to failure of venous valves, causing varicocele.
//////////////
Rx:
--------------------
Warn patient about possible decreased fertility.
If fertility is a concern to the pt -> semen analysis every 2 years.
Young pt (<= 20 yr) with clinically obvious hydrocele -> Surgery
Otherwise observation.
이 블로그 검색
2013년 6월 16일 일요일
2013년 6월 13일 목요일
Rheumatoid arthritis
- Rheumatoid Arthritis Criteria:
- -------------------------------
- Four of the following:
- 1 : Morning stiffness > 1 hr
- 3 : Affecting more than 3 joints
- <--> : symmetrical
- △
- | : involving hands and feet
- ▽
- (above 4 things for 6 weeks)
- R : Rheumatoid factor positive
- R : Rheumatoid nodules over extensor surfaces
- R : Radiographic changes
BPPV (Benign paroxysmal positional vertigo)
Background Knowledge:
-------------------------------------------------------
Semicircular canal has three components:
anterior(superior), posterior, lateral(horizontal) canal
Posterior canal BPPV — The Dix-Hallpike maneuver
--------------------------------------------------------------
Method:
- The patient's head is turned 45° towards the ear being tested.
- The head is supported, and then the patient is quickly lowered into the supine position with the head extending about 30° below the horizontal while remaining turned 45° towards the ear being tested.
- The head is held in this position and the physician checks for nystagmus.
- To complete the manoeuvre, the patient is returned to a seated position and the eyes are again observed for reversal nystagmus.
Interpretation (Positive Hallpike test):
Head is turned to the right, to test the right ear.
If the right ear is affected, nystagmus occurs as described below:
A: When the head is lowered 30 degree below the bed,
the fast phase of the nystagmus is upward , rotating toward the affected ear
B: When the patient is brought back to the sitting position,
the fast phase of the nystagmus is downward , rotating toward the affected ear
Anterior canal BPPV - The Dix-Hallpike maneuver
--------------------------------------------------------------
Method:
- same as posterior canal BPPV
Interpretation:
In positive Hallpike test, the nystagmus is downbeat and torsional(rotational), with the top of the eye torting away from the lower ear.
Treatment of Posterior or Anterior canal BPPV
--------------------------------------------------------------
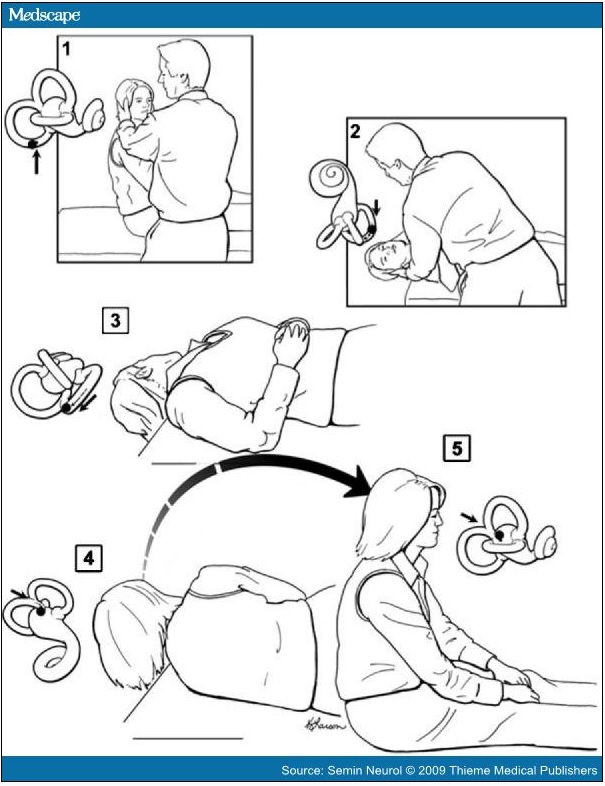
Two methods: Epley maneuver and Semont maneuver
Epley maneuver
/////////////////
Place the patient in a sitting position on the end of the examination table.
Rotate the head 45° towards the affected ear, then swiftly place the patient in a supine position with the head hanging 30° below the horizontal at the end of the examining table (Dix-Hallpike position).
Observe for nystagmus and hold the position for ~30 seconds after it stops.
The head is rotated 90° towards the opposite ear while maintaining the head hanging position.
Observe for nystagmus and hold the position for ~30 seconds after it stops.
Continue then to roll the whole patient another 90° towards the unaffected side until their head is facing 180° from the original Dix-Hallpike position. This change in position should take <3 to 5 seconds.
Observe for nystagmus and hold the position for ~30 seconds after it stops.
Then have the patient sit up. Upon sitting, there should be no vertigo or nystagmus in a successful manoeuvre, because the particles will have been cleared from the posterior semicircular canal back into the utricle.
If there is not paroxysmal nystagmus or symptoms during Dix-Hallpike positioning (Steps 1, 2) then there is a high likelihood of success.
/////////////////
Semont maneuver
////////////////
Sit the patient midway along the long side of an examination table, with their legs hanging over the edge.
Rotate the head 45° towards the unaffected side. While maintaining the head rotation, swiftly place the patient's upper body in a side-lying position on the affected side, with the head resting on the examination table and now facing upwards. This may induce nystagmus and vertigo because of particle movement towards the apex of the semicircular canal. Maintain this position until the vertigo and nystagmus stop (1 to 2 minutes).
Move the patient rapidly through the sitting position of step 1 and into the opposite side-lying position while maintaining the same head rotation, so that the head is resting on the examination table and now facing downwards. A nystagmus response in the same direction would indicate that the particles are exiting the semicircular canal. The transition from step 2 to 3 relies on inertia, and therefore it must be done very quickly. Maintain this position until the vertigo and nystagmus stop (1 to 2 minutes). Slowly return the patient to the sitting position of step 1.
Lateral(Horizontal) canal BPPV - Supine head turn maneuver
--------------------------------------------------------------
The nystagmus of horizontal canal BPPV, unlike that of posterior canal BPPV, is distinctly horizontal(moving to the left and or to the right, i.e. not up and down) and changes direction with changes in head position. There is no torsional(rotational) component.
The paroxysmal direction changing nystagmus may be either geotropic or apogeotropic.
Geotropic direction-changing positional nystagmus is right beating upon turning the head to the right and then left beating when turning the head back to the left side. (geotropic nystagmus = nystagmus "towards ground")
Conversely, the apogeotropic form indicates the nystagmus is right beating with turning to the left and left beating with turning to the right. (apogeotropic nystagmus = nystagmus "away from ground")
In geotropic nystagmus,
The downward ear, on the side where the nystagmus is more intense = the affected ear.
In apogeotrpic nystagmus,
The downward ear, on the side where the nystagmus is less intense = the affected ear.
{그냥 쉽게 병변 쪽으로 nystagmus 가 더 심하게 흘겨 본다고 보면 됨}
The latency is often brief, and the duration may be 15 to 60 seconds. This nystagmus appears less apt to fatigue with repeat
positioning than in cases of posterior canal BPPV; consequently, patients are more likely to become ill with attempts to fatigue this
form of BPPV.
(There is speculation that apogeotropic direction-changing nystagmus suggests cupulolithiasis, and geotropic nystagmus
suggests canalithiasis as the mechanism.)
Treatment of Lateral(Horizontal) canal BPPV
--------------------------------------------------------------
Lempert roll maneuver
////////////////////////
Lempert 360- (Barbeque) degree roll maneuver to treat horizontal canal BPPV. When the patient's head is positioned with the affected ear down, the head is then turned quickly 90 degrees toward the unaffected side (face up). A series of 90-degree turns toward the unaffected side is then undertaken sequentially until the patient has turned 360 degrees and is back to the affected ear-down position. From there, the patient is turned to the face-up position and then brought up to the sitting position. The successive head turns can be done in 15- to 20-second intervals even when the nystagmus continues. Waiting longer does no harm, but may lead to the patient developing nausea, and the shorter interval does not appear to detract from the effectiveness of the treatment.
////////////////////////
Gufoni maneuver
////////////////////////
(1) patient seated on the examination couch with both the legs hanging out from the same side, arms held close to the body, and
hands resting on the knees
(2) patient is then made to lie down on the uninvolved lateral side with a quick lateral movement and maintained in this position for 2
minutes until the end of evoked geotropic nystagmus
(3) quick 45° rotation of the head towards the floor, position being maintained for 2 minutes
(4) slow return back to the starting position
////////////////////////
Chracteristics of BPPV:
---------------------------------
- The latency, transience, and fatigability of the nystagmus
(latency - few seconds (2~5 sec)
transience - usu. lasts less than 30 sec
fatigability - nystagmus / diziness weakens with repeted maneuver)
- Typical mixed upbeat/downbeat + torsional(rotational) nystagmus
Characteristics of Central disorder:
---------------------------------
Latency - none
duration of nystagmus - greater than 1 minute
not-fatiguing
(videos:
Post/Ant canal BPPV
http://www.youtube.com/watch?v=59EIKztATiw
http://www.youtube.com/watch?v=LsPURdtMjac
Laterl canal BPPV
http://www.youtube.com/watch?v=iOJOArGmepM
http://balancemd.net/Horizontal_Canal_BPPV.html)
-------------------------------------------------------
Semicircular canal has three components:
anterior(superior), posterior, lateral(horizontal) canal
Posterior canal BPPV — The Dix-Hallpike maneuver
--------------------------------------------------------------
Method:
- The patient's head is turned 45° towards the ear being tested.
- The head is supported, and then the patient is quickly lowered into the supine position with the head extending about 30° below the horizontal while remaining turned 45° towards the ear being tested.
- The head is held in this position and the physician checks for nystagmus.
- To complete the manoeuvre, the patient is returned to a seated position and the eyes are again observed for reversal nystagmus.
Interpretation (Positive Hallpike test):
Head is turned to the right, to test the right ear.
If the right ear is affected, nystagmus occurs as described below:
A: When the head is lowered 30 degree below the bed,
the fast phase of the nystagmus is upward , rotating toward the affected ear
B: When the patient is brought back to the sitting position,
the fast phase of the nystagmus is downward , rotating toward the affected ear
Anterior canal BPPV - The Dix-Hallpike maneuver
--------------------------------------------------------------
Method:
- same as posterior canal BPPV
Interpretation:
In positive Hallpike test, the nystagmus is downbeat and torsional(rotational), with the top of the eye torting away from the lower ear.
Treatment of Posterior or Anterior canal BPPV
--------------------------------------------------------------
Two methods: Epley maneuver and Semont maneuver
Epley maneuver
/////////////////
Place the patient in a sitting position on the end of the examination table.
Rotate the head 45° towards the affected ear, then swiftly place the patient in a supine position with the head hanging 30° below the horizontal at the end of the examining table (Dix-Hallpike position).
Observe for nystagmus and hold the position for ~30 seconds after it stops.
The head is rotated 90° towards the opposite ear while maintaining the head hanging position.
Observe for nystagmus and hold the position for ~30 seconds after it stops.
Continue then to roll the whole patient another 90° towards the unaffected side until their head is facing 180° from the original Dix-Hallpike position. This change in position should take <3 to 5 seconds.
Observe for nystagmus and hold the position for ~30 seconds after it stops.
Then have the patient sit up. Upon sitting, there should be no vertigo or nystagmus in a successful manoeuvre, because the particles will have been cleared from the posterior semicircular canal back into the utricle.
If there is not paroxysmal nystagmus or symptoms during Dix-Hallpike positioning (Steps 1, 2) then there is a high likelihood of success.
/////////////////
Semont maneuver
////////////////
Sit the patient midway along the long side of an examination table, with their legs hanging over the edge.
Rotate the head 45° towards the unaffected side. While maintaining the head rotation, swiftly place the patient's upper body in a side-lying position on the affected side, with the head resting on the examination table and now facing upwards. This may induce nystagmus and vertigo because of particle movement towards the apex of the semicircular canal. Maintain this position until the vertigo and nystagmus stop (1 to 2 minutes).
Move the patient rapidly through the sitting position of step 1 and into the opposite side-lying position while maintaining the same head rotation, so that the head is resting on the examination table and now facing downwards. A nystagmus response in the same direction would indicate that the particles are exiting the semicircular canal. The transition from step 2 to 3 relies on inertia, and therefore it must be done very quickly. Maintain this position until the vertigo and nystagmus stop (1 to 2 minutes). Slowly return the patient to the sitting position of step 1.
Lateral(Horizontal) canal BPPV - Supine head turn maneuver
--------------------------------------------------------------
The nystagmus of horizontal canal BPPV, unlike that of posterior canal BPPV, is distinctly horizontal(moving to the left and or to the right, i.e. not up and down) and changes direction with changes in head position. There is no torsional(rotational) component.
The paroxysmal direction changing nystagmus may be either geotropic or apogeotropic.
Geotropic direction-changing positional nystagmus is right beating upon turning the head to the right and then left beating when turning the head back to the left side. (geotropic nystagmus = nystagmus "towards ground")
Conversely, the apogeotropic form indicates the nystagmus is right beating with turning to the left and left beating with turning to the right. (apogeotropic nystagmus = nystagmus "away from ground")
In geotropic nystagmus,
The downward ear, on the side where the nystagmus is more intense = the affected ear.
In apogeotrpic nystagmus,
The downward ear, on the side where the nystagmus is less intense = the affected ear.
{그냥 쉽게 병변 쪽으로 nystagmus 가 더 심하게 흘겨 본다고 보면 됨}
The latency is often brief, and the duration may be 15 to 60 seconds. This nystagmus appears less apt to fatigue with repeat
positioning than in cases of posterior canal BPPV; consequently, patients are more likely to become ill with attempts to fatigue this
form of BPPV.
(There is speculation that apogeotropic direction-changing nystagmus suggests cupulolithiasis, and geotropic nystagmus
suggests canalithiasis as the mechanism.)
Treatment of Lateral(Horizontal) canal BPPV
--------------------------------------------------------------
Lempert roll maneuver
////////////////////////
Lempert 360- (Barbeque) degree roll maneuver to treat horizontal canal BPPV. When the patient's head is positioned with the affected ear down, the head is then turned quickly 90 degrees toward the unaffected side (face up). A series of 90-degree turns toward the unaffected side is then undertaken sequentially until the patient has turned 360 degrees and is back to the affected ear-down position. From there, the patient is turned to the face-up position and then brought up to the sitting position. The successive head turns can be done in 15- to 20-second intervals even when the nystagmus continues. Waiting longer does no harm, but may lead to the patient developing nausea, and the shorter interval does not appear to detract from the effectiveness of the treatment.
////////////////////////
Gufoni maneuver
////////////////////////
(1) patient seated on the examination couch with both the legs hanging out from the same side, arms held close to the body, and
hands resting on the knees
(2) patient is then made to lie down on the uninvolved lateral side with a quick lateral movement and maintained in this position for 2
minutes until the end of evoked geotropic nystagmus
(3) quick 45° rotation of the head towards the floor, position being maintained for 2 minutes
(4) slow return back to the starting position
////////////////////////
Chracteristics of BPPV:
---------------------------------
- The latency, transience, and fatigability of the nystagmus
(latency - few seconds (2~5 sec)
transience - usu. lasts less than 30 sec
fatigability - nystagmus / diziness weakens with repeted maneuver)
- Typical mixed upbeat/downbeat + torsional(rotational) nystagmus
Characteristics of Central disorder:
---------------------------------
Latency - none
duration of nystagmus - greater than 1 minute
not-fatiguing
(videos:
Post/Ant canal BPPV
http://www.youtube.com/watch?v=59EIKztATiw
http://www.youtube.com/watch?v=LsPURdtMjac
Laterl canal BPPV
http://www.youtube.com/watch?v=iOJOArGmepM
http://balancemd.net/Horizontal_Canal_BPPV.html)
2013년 6월 11일 화요일
CXR - Dilated heart

Enlarged globular cardiac silhouette with cardiothoracic ratio of 58%. Right cardiac border forms a double contour; this usually suggests left atrial dilatation, but in this case it is caused by right atrial dilatation.
(reference: Circulation August 26, 2008 vol. 118 no. 9 e133-e135)
Subclinical Hyperthryoidism
Low TSH + Normal FT4 + Normal FT3 -> subclinical hyperthryoidism
studies lack, but hyperthyroidism treatment (antithyroid meds/radioactive iodine) probably helps against osteoporosis and cardiac arrhythmia.
Cause:
Exogenous - thyroid hormone tablet.
Endogenous - multinodular goiter, thyroid adenoma - are the most common cause of endogenous subclinical hyperthyroidism.
Rx:
TSH < 0.1 mU/ml -> treat the cause.
TSH 0.1~0.5
-> in elderly or high risk pt - treat the cause.
-> in low risk pt - observe. repeat blood test every 6 months.
studies lack, but hyperthyroidism treatment (antithyroid meds/radioactive iodine) probably helps against osteoporosis and cardiac arrhythmia.
Cause:
Exogenous - thyroid hormone tablet.
Endogenous - multinodular goiter, thyroid adenoma - are the most common cause of endogenous subclinical hyperthyroidism.
Rx:
TSH < 0.1 mU/ml -> treat the cause.
TSH 0.1~0.5
-> in elderly or high risk pt - treat the cause.
-> in low risk pt - observe. repeat blood test every 6 months.
UA/ Non-STEMI
Angina is considered to be unstable if it is prolonged (lasting more than 20 minutes), if it occurs at rest.
Unstable angina:
absence of biochemical evidence of myocardial damage
clinical findings of prolonged (>20 minutes) angina at rest
NSTEMI is distinguished from UA by the presence of elevated serum biomarkers. ST segment elevations and Q waves are absent in
both UA and NSTEMI. As a result, UA and NSTEMI are frequently indistinguishable at initial evaluation since an elevation in serum
biomarkers is usually not detectable for four to six hours after an MI, and at least 12 hours are required to detect elevations in all
patients.
DX:
----------
Cardiac biomarkers (troponin I or T, and creatine kinase-MB [CK-MB]) should be measured on presentation.
CK-MB has low sensitivity during early (<6 hours) or late (>36 hour) symptom onset and for minor damage.
CK-MB also has low specificity
Both troponin T (TnT) and troponin I (TnI) are more specific but have lower sensitivity for the very early detection of myocardial
necrosis. If the early (<6 hours from symptom onset) troponin test is normal, it should be repeated after 8 to 12 hours.
Troponin remains elevated up to 10 to 14 days after release.
ECG findings in UA/NSTEMI: normal or ST depression +- T wave inversion
A repeat ECG should be performed at 6 and 24 hours and if clinical status changes.
{즉,
Normal ECG -> repeat after 8 hrs.
Normal CK-MB, Trop I -> repeat after 8 hrs.
}
RX:
-----------
{
MONA
BS
invasive approach or non-invasive approach
}
MONA (aspirin 300 mg + clopidogrel 300 mg)
(antiplatelet continuation dose - aspirin 75 mg + clopidogrel 75 mg daily PO)
exclude use of errectile drugs (e.g.viagra) before using nitrate.
B(beta blocker) S(statin)
Invasive approach:
-PCI/CABG plus abciximab IVI
Non-invasive approach:
-Enoxaparin sodium 1 mg/kg SC 12hrly X 7 days plus abciximab IVI
An aggressive approach to reperfusion using PCI is best suited for patients with an elevated troponin level or a TIMI risk score ≥5 or
possibly other high-risk features. (See 'High-risk patient' below.) For patients at lower risk, approaches vary based upon hospital
protocol.
Fibrinolytic therapy is not beneficial in patients with a non-ST elevation ACS. (-> This is the difference between STEMI and Non-
STEMI) Therefore, thrombolytic therapy should NOT be administered to patients with UA or NSTEMI unless subsequent ECG
monitoring documents ST segment elevations that persist.
Unstable angina:
absence of biochemical evidence of myocardial damage
clinical findings of prolonged (>20 minutes) angina at rest
NSTEMI is distinguished from UA by the presence of elevated serum biomarkers. ST segment elevations and Q waves are absent in
both UA and NSTEMI. As a result, UA and NSTEMI are frequently indistinguishable at initial evaluation since an elevation in serum
biomarkers is usually not detectable for four to six hours after an MI, and at least 12 hours are required to detect elevations in all
patients.
DX:
----------
Cardiac biomarkers (troponin I or T, and creatine kinase-MB [CK-MB]) should be measured on presentation.
CK-MB has low sensitivity during early (<6 hours) or late (>36 hour) symptom onset and for minor damage.
CK-MB also has low specificity
Both troponin T (TnT) and troponin I (TnI) are more specific but have lower sensitivity for the very early detection of myocardial
necrosis. If the early (<6 hours from symptom onset) troponin test is normal, it should be repeated after 8 to 12 hours.
Troponin remains elevated up to 10 to 14 days after release.
ECG findings in UA/NSTEMI: normal or ST depression +- T wave inversion
A repeat ECG should be performed at 6 and 24 hours and if clinical status changes.
{즉,
Normal ECG -> repeat after 8 hrs.
Normal CK-MB, Trop I -> repeat after 8 hrs.
}
RX:
-----------
{
MONA
BS
invasive approach or non-invasive approach
}
MONA (aspirin 300 mg + clopidogrel 300 mg)
(antiplatelet continuation dose - aspirin 75 mg + clopidogrel 75 mg daily PO)
exclude use of errectile drugs (e.g.viagra) before using nitrate.
B(beta blocker) S(statin)
Invasive approach:
-PCI/CABG plus abciximab IVI
Non-invasive approach:
-Enoxaparin sodium 1 mg/kg SC 12hrly X 7 days plus abciximab IVI
An aggressive approach to reperfusion using PCI is best suited for patients with an elevated troponin level or a TIMI risk score ≥5 or
possibly other high-risk features. (See 'High-risk patient' below.) For patients at lower risk, approaches vary based upon hospital
protocol.
Fibrinolytic therapy is not beneficial in patients with a non-ST elevation ACS. (-> This is the difference between STEMI and Non-
STEMI) Therefore, thrombolytic therapy should NOT be administered to patients with UA or NSTEMI unless subsequent ECG
monitoring documents ST segment elevations that persist.
2013년 6월 8일 토요일
Asthma
=================
Asthma
=================
Symp:
SOB (in)
cough (물 out)
wheeze (공기 out)
inability to speak (소리 out)
Tests:
PEFR
Sats
+- ABG / CXR
Criteria:
mild: PEFR > 70% - dyspnoea only with exertion
moderate: PEFR 40~70 % - dyspnoea limits daily activity
severe: < 40 % - interferes conversation
(peadiatric crteria
PEFR is the same.
mild: talks in sentences
moderate: talks in phrases
severe: talks in words/ can't talk
)
Sat < 90 %
-> at least severe to life threatening asthma
Rx:
Oxygen
Inhaled Short-acting Beta2 agonists
Oral corticosteroid
Inhaled Anticholinergic
Magnesium
{데이빗 "배컴"
BACOM - Beta agonist, Anticholinergic, Corticosteroid, Magnesium
AA - Adrenaline, Antibiotics (adjuntive therapies)
}
///////
--mild--
-Salbutamol 2.5 ~ 5 mg nebulized every 20 min X 3
-Oral corticosteroid - prednisone 40 ~ 80 mg / day X 7 days
(
Pead dose:
Oral corticosteroid - prednisone 1mg/kg/day (max 40mg) (IV dose is the same)
)
--moderate to severe--
-Ipratropium bromide 0.5 mg nebulized in combination with salbutamol as above (every 20 min X 3)
-MgSO4 - 2 g IV over 20 min
---Life threatening ---
-IV hydrocortisone mg IVI 8 hrs (can be switched to oral as soon as possible)
-adjunct -
epinephrine: 0.01 mg/kg IMI as a single dose, if anaphylaxis suspected
antibiotics if infection suspected ( mycoplasma penumonia most common - erythromycin 50mg/kg/day in 4 divided doses)
///////
==================
Asthma
==================
criteria:
mild:
-FEV1 > 80 %
-symptom <= 2 per wk
-night symptom <= 2 per month
(mem tip 2, 2)
moderate:
-FEV1 60~80 %
-symptom daily
-night symptom > 1 per wk
(mem tip 1, 1)
severe:
-FEV1 < 60 %
DX:
Low in both FEV1/FVC and FEV1.
( FEV1/FVC < 80 % predicted
FEV1 < 80 % predicted )
FEV1 improves by 200 ml AND 12 % after bronchodilator.
Rx:
mild - short acting beta agnoist (e.g. salbutamol)
persistent mild - short acting beta agonist + corticosteroid inhaler
moderate - short acting beta agonist + corticosteroid inhaler + long acting beta agonist (e.g. salmeterol)
severe - short acting beta agonist + corticosteroid inhaler + long acting beta agonist (e.g. salmeterol) + oral corticosteroid
Asthma
=================
Symp:
SOB (in)
cough (물 out)
wheeze (공기 out)
inability to speak (소리 out)
Tests:
PEFR
Sats
+- ABG / CXR
Criteria:
mild: PEFR > 70% - dyspnoea only with exertion
moderate: PEFR 40~70 % - dyspnoea limits daily activity
severe: < 40 % - interferes conversation
(peadiatric crteria
PEFR is the same.
mild: talks in sentences
moderate: talks in phrases
severe: talks in words/ can't talk
)
Sat < 90 %
-> at least severe to life threatening asthma
Rx:
Oxygen
Inhaled Short-acting Beta2 agonists
Oral corticosteroid
Inhaled Anticholinergic
Magnesium
{데이빗 "배컴"
BACOM - Beta agonist, Anticholinergic, Corticosteroid, Magnesium
AA - Adrenaline, Antibiotics (adjuntive therapies)
}
///////
--mild--
-Salbutamol 2.5 ~ 5 mg nebulized every 20 min X 3
-Oral corticosteroid - prednisone 40 ~ 80 mg / day X 7 days
(
Pead dose:
Oral corticosteroid - prednisone 1mg/kg/day (max 40mg) (IV dose is the same)
)
--moderate to severe--
-Ipratropium bromide 0.5 mg nebulized in combination with salbutamol as above (every 20 min X 3)
-MgSO4 - 2 g IV over 20 min
---Life threatening ---
-IV hydrocortisone mg IVI 8 hrs (can be switched to oral as soon as possible)
-adjunct -
epinephrine: 0.01 mg/kg IMI as a single dose, if anaphylaxis suspected
antibiotics if infection suspected ( mycoplasma penumonia most common - erythromycin 50mg/kg/day in 4 divided doses)
///////
==================
Asthma
==================
criteria:
mild:
-FEV1 > 80 %
-symptom <= 2 per wk
-night symptom <= 2 per month
(mem tip 2, 2)
moderate:
-FEV1 60~80 %
-symptom daily
-night symptom > 1 per wk
(mem tip 1, 1)
severe:
-FEV1 < 60 %
DX:
Low in both FEV1/FVC and FEV1.
( FEV1/FVC < 80 % predicted
FEV1 < 80 % predicted )
FEV1 improves by 200 ml AND 12 % after bronchodilator.
Rx:
mild - short acting beta agnoist (e.g. salbutamol)
persistent mild - short acting beta agonist + corticosteroid inhaler
moderate - short acting beta agonist + corticosteroid inhaler + long acting beta agonist (e.g. salmeterol)
severe - short acting beta agonist + corticosteroid inhaler + long acting beta agonist (e.g. salmeterol) + oral corticosteroid
피드 구독하기:
글 (Atom)